The identification of the predictors of locomotion ability could help professionals select variables to be considered during clinical evaluations and interventions.
ObjectiveTo investigate which impairment measures would best predict locomotion ability in people with chronic stroke.
MethodsIndividuals (n=115) with a chronic stroke were assessed. Predictors were characteristics of the participants (i.e. age, sex, and time since stroke), motor impairments (i.e. muscle tonus, strength, and motor coordination), and activity limitation (i.e. walking speed). The outcome of interest was the ABILOCO scores, a self-reported questionnaire for the assessment of locomotion ability, designed specifically for individuals who have suffered a stroke.
ResultsAge, sex, and time since stroke did not significantly correlate with the ABILOCO scores (−0.07<ρ<0.05; 0.48<p<0.99). Measures of motor impairments and walking speed were significantly correlated with the ABILOCO scores (−0.25<r<0.57; p<0.001), but only walking speed and strength were kept in the regression model. Walking speed alone explained 35% (F=55.5; p<0.001) of the variance in self-reported locomotion ability. When strength was included in the model, the explained variance increased to 37% (F=31.4; p<0.001).
ConclusionsWalking speed and lower limb strength best predicted locomotion ability as perceived by individuals who have suffered a stroke.
Recent data indicate that over 30 million people in the world have survived a stroke, which is the leading cause of long-term disability.1,2 Following a stroke, a myriad of personal characteristics and clinical impairments have the potential to interfere with the performance of daily life activities,3 such as locomotion. Locomotion refers to the individuals’ abilities to effectively move in their environment and includes activities, such as walking, running, turning, and managing stairs.3 Decreased locomotion ability has been associated with restrictions in leisure activities and community participation.4,5
Nowadays, great emphasis has been given to self-reported measures, since they provide the patients’ perspectives on their daily activities.6 However, since locomotion ability is a wider construct, compared to walking ability, the difficulty of deciding on a proper instrument may explain the small number of studies that examined factors related to locomotion ability after stroke. The ABILOCO questionnaire is a self-reported measure, specific for individuals with stroke for the measurement of locomotion ability, which explores a representative repertoire of activities in the home and community environments.4 Previous studies have reported appropriate measurement properties of the ABILOCO questionnaire, such as test-retest reliability, concurrent validity, linearity, unidimensionality, and reproducibility.4,7,8 Recently, this questionnaire was translated, cross-culturally adapted, and validated to the Brazilian Portuguese language.9
Many factors, such as age, sex, muscle strength, muscle tone, motor coordination, balance, and walking speed, have the potential to interfere with locomotion ability.3 There have been two studies,7,10 which investigated the relationships between locomotion ability (i.e., ABILOCO scores) and measures of motor impairments (e.g., balance) and activity limitations (e.g., walking, mobility) after stroke.7,10 However, studies which investigated the potential measures that could predict locomotion ability, including the main impairments found after a stroke, such as weakness and motor coordination deficits, were not found. Previous studies have already described that both measures of muscle strength and motor coordination are strong predictors of the ability to use the paretic upper limb in daily activities.11–13 On the other hand, the designs of the studies and their methodological characteristics prevent appropriate conclusions regarding the predictors of lower-limb activities after stroke. The identification of these factors could help professionals to select variables to be considered during clinical evaluations and interventions.
According to the International Classification of Functioning, Disability and Health, mobility of individuals with disabilities is influenced by the interactions between their health condition and the personal and environmental contexts in which they conduct their lives.3 However, much of the available evidence regarding movement and mobility in patients with stroke has focused on impairments in body structure and function that contribute to and/or influence activities. Appropriate attention has not been given to the contextual factors or personal characteristics that affect mobility and locomotion. Therefore, the purpose of this study was to investigate which measures would best predict self-reported locomotion ability, assessed by the ABILOCO questionnaire, in people with chronic stroke. The specific research questions were: What were the magnitudes and directions of the relationships between personal characteristics and clinical measures, and locomotion ability following a stroke? Which of these measures would best predict locomotion ability following a stroke?
MethodsParticipantsFor this exploratory study, community-dwelling people with stroke were recruited by means of advertisements and by screening out-patient clinics in public hospitals and rehabilitation centers, from March 2013 to December 2014. People were included if they were ≥20 years of age and at least six months after the onset of an ischemic or hemorrhagic stroke; had weakness and/or increased tonus of the ankle plantar flexor muscles, as determined by 15% strength differences between the paretic and non-paretic limbs14 and/or scores different from zero on the Modified Ashworth Scale15; and had no cognitive impairments, as determined by the following education-adjusted cut-off scores on the Mini-mental state examination: 18/19 for the individuals with illiteracy and 24/25 for those with basic education.16 Individuals were excluded if they had any cardiac, musculoskeletal, or other non-stroke related conditions, which could prevent measurement.
ProceduresBefore data collection, eligible participants were informed about the objectives of the study and provided written consent, based upon previous approval from the Institutional ethical review board of the Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil, Ethical Review Board (#CAAE 06609312.0.0000.5149). Demographic and clinical data were obtained by interviews, followed by clinical measurements of motor impairments, walking speed, and locomotion ability.
OutcomesThe potential predictors were characteristics of the participants (i.e. age, sex, time since stroke), clinical measures of motor impairments (i.e. muscle tone, strength, and motor coordination) and activity limitation (i.e. walking speed). The characteristics of the participants were directly asked to the participants or caregivers, whereas clinical measures of motor impairments and walking speed were collected by well-trained physical therapists on one day in a laboratory setting, as follows:
The tonus of the paretic ankle plantar flexors muscles was measured using the modified Ashworth Scale15 and reported on a 6-point scale that ranges from zero (i.e. no increase in muscle tone) to four (i.e. paretic limb rigid in flexion or extension). Measurements were taken with the participants lying in the supine position, with their lower limb completely relaxed. This scale is widely used within a clinical context and has been shown to be adequately reliable for individuals who have suffered a stroke.15
Maximal isometric strength of the paretic hip flexor and knee flexor/extensor muscles was measured using the hand-held dynamometer (Microfet 2MT, Hoggan Health Industries, West Jordan, UT). The strength measures of the three muscle groups were summed and reported, in kilograms of force (kgf). All strength measurements were taken with the participants lying in the supine position, with their lower limb to be tested placed on a stool at 90° of hip and knee flexion.17 The participants were instructed to push as hard as they could against the dynamometer for 3–4s.18
Motor coordination of the paretic lower limb was measured using the lower extremity motor coordination test (i.e. LEMOCOT) and reported as number of touched targets. This test has excellent measurement properties, when applied to people who have suffered a stroke19 and proved to be the most suitable lower-limb motor coordination test for this population.20 The participants performed the LEMOCOT three times with their paretic lower limbs, and the mean values were registered for analyses.19,20 To perform the LEMOCOT, the participants sat on an adjustable chair with their feet resting flat on a thin rigid piece of foam, heels on the proximal target, and knees at 90° of flexion. Then, after a familiarization trial, they were instructed to alternately touch the proximal and distal targets placed 30cm apart with their big toe, for 20s. They were instructed not to sacrifice the accuracy of the touches, nor the quality of the movement, to increase speed.20
Walking speed was measured using the 10m Walk Test, and reported in m/s. The participants were instructed to walk at their most “comfortable speed” along a 14-m hallway, using their usual assistive devices or orthoses.21 The time to cover the central 10m was recorded once with a digital stopwatch after familiarization, as one trial has been shown to generate reliable results with people who have suffered a stroke.22
The outcome of interest, (i.e. the primary outcome), was locomotion ability, measured using the ABILOCO questionnaire, and reported as logits, the unit of measure of Rasch analysis. It is a stroke-specific questionnaire, which contains 13 items related to locomotion activities.4 Participants were asked to estimate their ability to perform the locomotion activities, which were rated as 0=impossible or 1=possible. The activities, which were not attempted after the stroke, were inserted as missing responses.4 The responses were submitted on-line to Rasch analysis, and results were used as the outcome measure.
Sample sizeBased upon the following formula recommended by Tabachnick and Fidell23: (n≥104+M), where M is the number of predictors, a sample of at least 111 participants would be required to perform the regression analysis.
Statistical analysesDescriptive statistics and tests for normality (Kolmogorov–Smirnov) were calculated for all outcome variables. Spearman correlation coefficients (two-tailed) were calculated to explore the relationships between the predictors and self-reported locomotion ability (ABILOCO scores). The strength of the relationships was classified as low (r<0.30), moderate (0.30<r<0.50), and high (>0.50).24 Although the variables were non-normally distributed, Willian et al. (2013) argued that multiple regression did not require that the predictor and/or response variables should be normally distributed.25 In reality, only the assumption of normally distributed errors is relevant to multiple regression.25 Thus, a step-wise multiple linear regression analysis was used to identify which measures, (i.e., age, sex, time since stroke, muscle tonus, strength, motor coordination, and walking speed) would significantly explain locomotion ability. Further, the distribution of the residuals was investigated to determine how well they fit the assumption of normally distributed errors for the model under consideration.25 All analyses were performed with the SPSS statistical software 23.0 for Windows, with a significance level of 5% and a power of at least 80%.
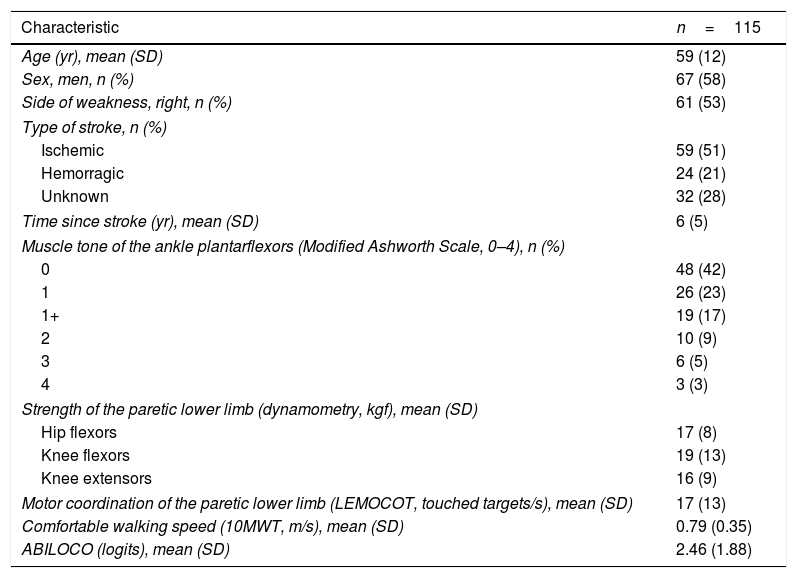
ResultsA total of 115 individuals, 67 men and 48 women, with a mean age of 59 (SD: 12) years and a mean time since the onset of the stroke of 6 (SD: 5) years, participated in the study. There was no missing data. Their characteristics are summarized in Table 1.
Characteristics of the participants in a study to look at locomotion using the ABILOCO questionaire.
| Characteristic | n=115 |
|---|---|
| Age (yr), mean (SD) | 59 (12) |
| Sex, men, n (%) | 67 (58) |
| Side of weakness, right, n (%) | 61 (53) |
| Type of stroke, n (%) | |
| Ischemic | 59 (51) |
| Hemorragic | 24 (21) |
| Unknown | 32 (28) |
| Time since stroke (yr), mean (SD) | 6 (5) |
| Muscle tone of the ankle plantarflexors (Modified Ashworth Scale, 0–4), n (%) | |
| 0 | 48 (42) |
| 1 | 26 (23) |
| 1+ | 19 (17) |
| 2 | 10 (9) |
| 3 | 6 (5) |
| 4 | 3 (3) |
| Strength of the paretic lower limb (dynamometry, kgf), mean (SD) | |
| Hip flexors | 17 (8) |
| Knee flexors | 19 (13) |
| Knee extensors | 16 (9) |
| Motor coordination of the paretic lower limb (LEMOCOT, touched targets/s), mean (SD) | 17 (13) |
| Comfortable walking speed (10MWT, m/s), mean (SD) | 0.79 (0.35) |
| ABILOCO (logits), mean (SD) | 2.46 (1.88) |
LEMOCOT, lower extremity motor coordination test; 10MWT, 10-meter walk test; kgf, kilograms of force; SD, standard deviation, m/s: meters per second; logits, locomotion ability; LEMOCOT, lower extremity motor coordination test.
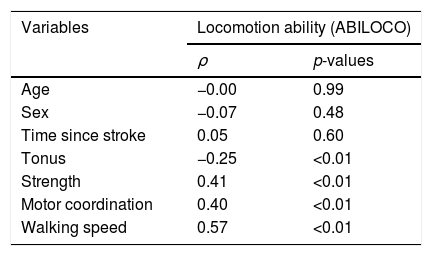
Table 2 provides the correlation coefficients between all selected measures and locomotion ability. All clinical measures of motor impairments (i.e., muscle tonus, strength, and motor coordination) and activity limitation (i.e. walking speed) were significantly correlated with locomotion ability (p<0.05). Regarding the motor impairments, the correlation with the tonus of the ankle plantar flexor muscles (i.e. Modified Asworth scores) was negative and of low magnitude (ρ=−0.25); positive and of moderate magnitude (ρ=0.41) with strength; and positive and of moderate magnitude (ρ=0.40) with motor coordination (i.e. LEMOCOT scores). The correlation between walking speed (i.e. 10 meter walk test – 10MWT) and locomotion ability was positive and of high magnitude (ρ=0.57). No significant associations were found between locomotion ability and any personal characteristics of the participants (−0.07<ρ<0.05; 0.48<p<0.99).
Spearman correlation coefficients (ρ) and statistical significance (p-values) between the selected variables and self-reported measure of locomotion ability (ABILOCO questionnaire).
| Variables | Locomotion ability (ABILOCO) | |
|---|---|---|
| ρ | p-values | |
| Age | −0.00 | 0.99 |
| Sex | −0.07 | 0.48 |
| Time since stroke | 0.05 | 0.60 |
| Tonus | −0.25 | <0.01 |
| Strength | 0.41 | <0.01 |
| Motor coordination | 0.40 | <0.01 |
| Walking speed | 0.57 | <0.01 |
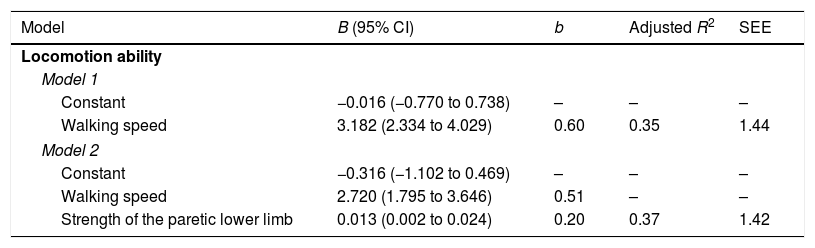
All significantly correlated variables (i.e. muscle tonus, strength, motor coordination, and walking speed), were included in the regression analysis as potential predictors of locomotion ability. However, only walking speed and strength reached significance (p<0.01) and, consequently, were kept in the model (Table 3). Walking speed alone explained 35% (F=55.5; p<0.001) of the variance in the ABILOCO scores. When strength was included in the model, the explained variance increased to 37% (F=31.4; p<0.001). Finally, the residual analysis from the regression model demonstrated a normal distribution (p>0.05), which fit the assumption of normally distributed errors for the model under consideration.
Results of the regression analysis regarding the potential predictors of self-reported locomotion ability (ABILOCO questionnaire) (n=115).
| Model | B (95% CI) | b | Adjusted R2 | SEE |
|---|---|---|---|---|
| Locomotion ability | ||||
| Model 1 | ||||
| Constant | −0.016 (−0.770 to 0.738) | – | – | – |
| Walking speed | 3.182 (2.334 to 4.029) | 0.60 | 0.35 | 1.44 |
| Model 2 | ||||
| Constant | −0.316 (−1.102 to 0.469) | – | – | – |
| Walking speed | 2.720 (1.795 to 3.646) | 0.51 | – | – |
| Strength of the paretic lower limb | 0.013 (0.002 to 0.024) | 0.20 | 0.37 | 1.42 |
B, regression coefficients; CI, confidence interval; b, standardized regression coefficient; R2, coefficient of determination; SEE, standard error of the estimate.
This study explored the relationships between a range of commonly-collected measures, which included personal characteristics and main clinical measures of motor impairments (such as tonus, strength, and motor coordination), activity limitation (i.e. walking speed), and self-reported locomotion ability in ambulatory people with chronic stroke. Moreover, this study also planned to identify which of the measures would significantly predict locomotion ability. The results revealed that all measures of motor impairments (i.e. muscle tonus, strength, and motor coordination) and activity limitation were significantly correlated with locomotion ability. However, only measures of walking speed and strength were kept in the regression model and explained 37% of the variance in locomotion ability. Age, sex, and time since stroke were not correlated with locomotion and may not influence the prognosis of recovery in individuals with chronic stroke. Therefore, the results reinforced the need to target modifiable factors, such as motor impairments (e.g. strength and motor coordination) and walking limitations during rehabilitation to improve locomotion ability following a stroke.
The findings of the present study demonstrated correlations of low to moderate magnitudes between locomotion ability and measures of motor impairments, (i.e., muscle tonus, strength and motor coordination). Although previous studies have already suggested that motor impairments are important contributors to locomotion ability after stroke,26–29 their understanding of locomotion ability was restricted to the walking component. Although walking is an important ability to be considered during rehabilitation interventions, locomotion ability covers an extensive repertoire of other activities, such as ascending stairs, stepping over obstacles, and turning.4
Two previous studies, with small samples (i.e. less than 35 participants), which explored associations between measures of motor impairments and locomotion after stroke,30,31 found similar results. One study indicated that locomotion ability was associated with total lower-limb muscle strength, (i.e., sum of the strength of the hip flexors, knee extensors and ankle dorsiflexors) (r=0.62, p<0.01), but was not associated with hypertonia.31 The other study indicated that locomotion was also associated with the strength of hip abductors (r=0.34, p=0.04).30 The results of the present study strengthen the evidence by investigating a large sample (n=115) and demonstrating that not only strength, but also motor coordination is associated with locomotion ability following a stroke.
In addition, our results demonstrated a correlation of high magnitude between locomotion ability and walking speed. The regression analysis, which included seven predictors that could potentially explain locomotion ability (i.e. age, sex, time since stroke, muscle tonus, strength, motor coordination, and walking speed), revealed that walking speed alone explained 35% of the variance in the ABILOCO scores. The results are in accordance with a previous trial, which indicated that locomotion ability was associated with walking speed (r=0.75, p<0.01) and walking distance (r=0.76, p<0.01).10 Therefore, interventions aimed at improving walking speed, such as treadmill training, body-weight support training, cueing of cadence, and virtual reality,32–34 and increasing the intensity of walking practice should be encouraged during rehabilitation, as they may have an impact on locomotion ability.35 Previous studies have demonstrated that better locomotion ability is associated with improved community ambulation and increased social participation.5,36 It is important to highlight that the mean time since the onset of the stroke in the present study was six years, and other factors, such as the ability to control the trunk, sitting balance, and functional status might be related to locomotion ability in individuals at the initial post-stroke phases (i.e. less than six months).37,38
Although the contribution of lower-limb strength was significant, it added only 2% to the explained variance in perceived locomotion ability. The fact that other muscle groups, such as hip extensors and plantar flexors, were not evaluated may have introduced some bias in the results. However, a recent study indicated that the strength of the knee extensor muscles reflected global lower-limb strength after stroke, which suggests that the results obtained in the present study were credible.39
This study has both strengths and limitations. The two major strengths are the large sample and the innovation of examining the two main impairments found after a stroke, such as weakness and motor coordination deficits, as potential predictors of self-reported locomotion ability after a stroke. Previous studies30,31,36,38 did not include the main negative motor impairments following upper motor neuron damage that mostly contribute to disability, (i.e., weakness and lack of motor coordination). In addition, the ABILOCO questionnaire offered additional strengths over other questionnaires, since it was originally constructed based upon the Rasch model, which allowed for the conversion of ordinal scores into linear measures.4 Linear measures offer more scientifically robust and clinically significant results, than ordinal ones and allow for correct inferences from direct inter- or intra-individual comparisons.40 However, this study was not without limitations. Although the sample was broad and drawn from various settings, it was not randomly selected and may not, therefore, be fully representative of the stroke population. Since the recruitment was conducted on a volunteer basis, those, who agreed to participate, may differ from those in the general community. In addition, only three lower limb muscle groups were evaluated and included as predictors, which may have underestimated the contribution of strength to locomotion. Future studies are recommended to include not only measures of strength of multiple lower-limb muscles and balance measurement, but also environmental factors to better clarify their contribution to self-reported locomotion ability. Finally, although self-perceived measures have the advantage of capturing an average performance in long periods of time, (i.e., the measurement does not only represent what the individual is able to perform during the test in a standardized environment), they are more susceptible to under or overestimation of actual patients’ performance.
ConclusionThe findings of the present study demonstrated that muscle tonus & strength, motor coordination, and walking speed were significantly correlated with self-reported locomotion ability in ambulatory people with a chronic stroke. However, only walking speed and strength measures explained the variance in locomotion ability. These findings suggest that perceived locomotion ability following a stroke may be increased if attention is focused on improving walking speed.
FundingThis research was supported by the Brazilian Funding Agencies: CAPES (code #001), CNPq (#304430/2014-0), and FAPEMIG (PPM-00082-16).
Conflicts of interestThe authors declare no conflicts of interest.
Brazilian Government Funding Agencies (CNPq and FAPEMIG) for the financial support.