The purpose of this review was to identify doses of exercise therapy associated with greater treatment effect sizes in individuals with common musculoskeletal disorders of the foot and ankle, namely, achilles tendinopathy, ankle sprains and plantar heel pain.
MethodsAMED, EMBASE and MEDLINE were searched from 2005 to August 2017 for randomized controlled trials related to exercise for these three diagnoses. The Physiotherapy Evidence Database scale was used for methodological quality assessment. Exercise dosing variables and outcome measures related to pain and function were extracted from the studies, and standardized mean differences were calculated for the exercise groups.
ResultsFourteen studies met the final inclusion. A majority of the studies showed large effects and two small trends were identified. Patients with plantar heel pain may benefit more from a daily home exercise program than two supervised visits per week (SMD=3.82), but this recommendation is based on weak evidence. In achilles tendinopathy, a relationship was also seen when sets and repetitions of eccentric exercise were performed as tolerated (SMD=1.08 for function, −1.29 for pain).
ConclusionsSession duration, frequency, total number of visits, and overall length of care may all be dosing variables with limited value for determining effective exercise prescription. However, the limited number of studies prevents any definitive conclusions. Further investigation is warranted to improve our understanding of the influence exercise dosing has on treatment effect sizes. Future randomized controlled trials comparing specific exercise dose variables should be conducted to clarify the impact of these variables.
Exercise therapy is often prescribed to treat musculoskeletal disorders of the lower extremity, and recommended in many clinical practice guidelines and systematic reviews.1–19 However, the amount of exercise performed and the specific relationship between dosing parameters and health benefits has not yet been determined. Therapeutic exercise for musculoskeletal disorders is the most commonly used intervention by physical therapists, above manual therapy, neuromuscular re-education and even modalities. However, the specific dosing varies greatly, and the definition of dose is poorly defined.20,21 Dose can refer to the total number of exercise sessions over a given period of time, the frequency of those sessions, or the time spent in each of those sessions. It is more frequently thought of as the repetitions, sets, number of total exercises, and progression of exercise. While there is evidence that exercise therapy is effective for many of these lower extremity disorders,22–24 there are few studies investigating the optimal dosing parameters associated with the best outcomes.
The American College of Sports Medicine (ACSM) has provided some general guidelines for exercise prescription, but they are clear in stating that it should be personalized for each individual.25 Little work has been done to determine if these guidelines align with the exercise prescribed in clinical trials for patients with lower extremity musculoskeletal disorders, or if the use of these guidelines results in favorable outcomes. Although the authors of the ACSM guidelines state that these recommendations may also apply to individuals with disabilities or chronic diseases, the guidelines were targeted to individuals looking to improve their overall health instead of those recovering from a musculoskeletal injury.25 Identification of optimal exercise dosing has the potential to improve outcomes and accelerate recovery during physical rehabilitation. In addition, identification of optimal dosing can help physical therapists provide efficient treatments, align with clinical practice guidelines and standardize dose in clinical trials.
In the lower extremity, the majority of research related to exercise dose is for hip and knee osteoarthritis.23,26,27 To the knowledge of the authors, there are no studies investigating the impact of specific dosing variables on foot and ankle disorders. Three common disorders of the foot and ankle, achilles tendinopathy (AT), ankle sprains, and plantar heel pain, are frequently managed with exercise.1,28–31 A recent editorial on AT and eccentric exercise highlighted the need for further trials investigating optimal exercise dosage.32 A common dose prescribed for patients with AT is three sets of 15 repetitions two times per day seven days per week with eccentric exercise as a home exercise program (HEP).6,8–10,12 Beyer and colleagues used this same prescription, and saw large effects related to pain and function.6 Yu et al.,13 on the other hand, used eccentric exercise three times per week and showed only medium effect sizes. These groups had different frequencies of intervention and total number of overall sessions. Hence, optimal outcomes may be related more to dosing of an exercise rather than the type of exercise. For patients with ankle sprains, there have been a wide variety of different exercise programs showing favorable results, but none of these have measured the impact of dosing on outcomes.28 Lastly, plantar heel pain has very limited evidence for the use of exercise as an effective intervention, and dosing information is highly lacking.30
When determining the value of exercise, it is important that clinicians understand the influence that effect size may have on clinical decision making. Traditionally, results are provided based on statistical significance, using p-values, which do not quantify the magnitude of difference between interventions like effect sizes do.33–35 Statistically significant improvement does not always mean there have been clinically important changes, and therefore results from clinical trials are often difficult to integrate into practice.33 Using effect sizes, clinicians can determine which interventions have the greatest impact on improving patient outcomes.36 For example, using the same type of eccentric exercises, Rompe and colleagues10 showed large effects on the Victorian Institute of Sports Assessment (VISA), whereas Stevens and Tan12 exhibited a medium effect size on the VISA. Although both were shown to be significantly effective, the magnitude of the effectiveness was higher in one group, and the dosing of exercise was different between groups. It would be valuable for clinicians to know which dosing variables are associated with larger treatment effect sizes.
There is much variation in the dosing of prescribed exercise for foot and ankle disorders; hence, the purpose of this systematic review was to identify specific exercise dosing variables that were related to improved outcomes in pain and/or function in patients with foot and ankle disorders. The secondary purpose was to categorize the dosing variables based on their effect size.
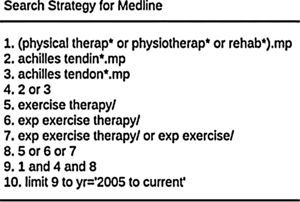
Materials and methodsSearch strategyThe Allied and Complementary Database (AMED), EMBASE and MEDLINE databases were used to identify relevant clinical trials that utilized therapeutic exercise in managing patients with achilles tendinopathy, ankle sprains and plantar heel pain. Studies were included if they: (1) were peer reviewed; (2) were a randomized controlled trial; (3) used therapeutic exercise as a primary intervention independently without a related intervention, such as a modality or manual therapy; and (4) were published from 2005 to August 2017. Studies were excluded if they: (1) were not published or translated in the English language; (2) did not include an outcome measure for pain and/or function. Because there are a large number of studies related therapeutic exercise and these disorders, the date range for the searches was limited from 2005 to August 2017 in order to include more recent evidence. The search for AT was performed using combinations of the following words and the Boolean operators of AND and OR: physical therapy, physiotherapy, rehabilitation, exercise, exercise therapy, achilles tendon, achilles tendinopathy, achilles tendonopathy, ankle sprain, acute ankle sprain, lateral ankle sprain, heel pain, plantar heel pain, posterior heel pain, plantar fasciitis, plantar fasciosis. Inclusion of exercise and exercise therapy in the searches for ankle sprains and plantar heel pain led to results that were too specific, so these terms were excluded for those two diagnoses in order to increase sensitivity. The appendix provides an example of one of the search strategies for achilles tendinopathy.
Study selection and data extractionThe studies, including titles and abstracts, identified by the searches were screened by two reviewers (JY and RD). Eligible full text studies were retrieved and screened again by the same reviewers. Any uncertainty in eligible studies was resolved by consensus discussion. To be as inclusive as possible, reference lists of the identified studies were manually checked for inclusion.
Data were extracted from the studies by one author (JY), including exercise type, single session duration, frequency of intervention, total number of sessions, duration of care, follow up time frame, outcome measures assessing pain and/or function, and the means and standard deviations associated with the extracted outcome measures.
Operational definitions for exercise type, single session duration, frequency of intervention, total number of sessions, duration of care and follow-up time frame were formalized for consistency. Table 1 provides the operational definitions.
Definitions of dosing variables.
| Dosing variable | Operational definition |
|---|---|
| Exercise type | Activity performed by a patient that was prescribed by a healthcare provider, and required physical effort with the intention of improving overall health and fitness.23,28 Can include aerobic activity, strengthening, stretching, balance or proprioceptive exercises. |
| Single session duration | Amount of time spent in one single exercise session, either supervised by a healthcare provider or as a HEP. |
| Frequency | How often the individual performed supervised exercise intervention or HEP. |
| Total number of sessions | Number of exercise sessions, supervised or HEP, that were performed over the duration of the study. |
| Duration of care | Number of days an individual performed supervised exercise or a HEP. |
| Follow-up time frame | Length of time, in days or weeks, between the initial exercise intervention and the final follow-up time frame. |
The standardized mean difference (SMD) was used to calculate the magnitude of effect. The values at baseline and follow-up time frame were used in order to provide the longest available follow-up time frame. The benchmarks from Cohen et al.37 (0.2 small; 0.5 medium; 0.8 large) were used to determine effect size. Table 2 provides the exercise type, dosing variables and SMDs for AT, ankle sprains and plantar heel pain. Meta-analysis was deemed inappropriate due to the heterogeneity of dosing variables and outcome measures.
Dosing variables and effect sizes for studies.
| Study | Exercise type | Single session duration | Frequency | Total number of sessions | Duration of care | Follow-up time frame | Standardized mean difference (calculated for time frame of study) | Magnitude of effect |
|---|---|---|---|---|---|---|---|---|
| Achilles tendinopathy | ||||||||
| Beyer et al.6 (eccentric) | Eccentric unilateral loading of the lower extremity while standing on a step with knee flexed and knee extended | 22min | 2×/day 7 days/week HEP | 168 | 12 weeks | 52 weeks | VISA SMD=1.40 VAS during running SMD=−1.51 | Large Large |
| Beyer et al.6 (heavy slow resistance) | 3 exercises on resistance equipment: heel rises with extended knee in leg press, heel raises with flexed knee in leg press and heel raises with extended knee standing on disk weight with forefoot and barbell on shoulders; decreasing repetitions and increasing load weekly | Variable | 3×/week HEP | 36 | 12 weeks | 52 weeks | VISA SMD=2.48 VAS during running SMD=−2.46 | Large Large |
| Rompe et al.8 | Standing eccentric exercises for gastronemius/soleus with knee flexed and extended | Not reported | 2×/day 7 days/week HEP | 168 | 12 weeks | 16 weeks | VISA SMD=1.61 | Large |
| Rompe et al.9 | Standing eccentric exercises for gastronemius/soleus with knee flexed and extended | Not reported | 2×/day 7 days/week HEP | 168 | 12 weeks | 16 weeks | VISA SMD=1.03 | Large |
| Rompe et al.10 | Standing eccentric exercises for gastronemius/soleus with knee flexed and extended | Not reported | 2×/day 7 days/week HEP | 168 | 12 weeks | 16 weeks | VISA SMD=1.47 | Large |
| Silbernagel et al.11 | Unilateral and bilateral eccentric and fast-bounding toe raises | Not reported | 1×/day HEP | Varied | 6 months | 12 months | VISA SMD=1.95 VAS SMD=−1.40 | Large Large |
| Stevens and Tan12 (as tolerated group) | Alfredson et al. protocol for eccentric heel drop exercises done for tolerable number of repetitions with knee flexed and with knee extended | Not reported | 2×/day 7 days a week HEP | 84 | 6 weeks | 6 weeks | VISA SMD=1.08 VAS SMD=−1.29 | Large Large |
| Stevens and Tan12 (standard treatment) | Alfredson et al. protocol for eccentric heel drop exercises done for 3 sets of 15 repetitions with knee flexed and with knee extended | Not reported | 2×/day 7 days a week HEP | 84 | 6 weeks | 6 weeks | VISA SMD=0.78 VAS SMD=−0.71 | Medium Medium |
| Yu et al.13 (eccentric) | Bicycle warm-up and cool down followed by eccentric exercise for heel raises with added resistance weekly | 50min | 3×/week supervised | 24 | 8 weeks | 8 weeks | VAS SMD=−5.12 Total Balance Index SMD=−3.98 | Large Large |
| Yu et al.13 (concentric) | Bicycle warm-up and cool down followed by concentric exercise for heel raises and stretching for knee flexion and extension | 50min | 3×/week supervised | 24 | 8 weeks | 8 weeks | VAS SMD=−3.13 Total Balance Index SMD=−0.52 | Large Medium |
| Ankle sprains | ||||||||
| Bassett and Prapavessis14 (clinic) | Range of motion, stretching and strengthening exercises for the lower extremity | Not reported | Varied; dependent on ability to advance with supervised program and HEP | Varied; average was 7.64 | Varied; dependent on patient recovery | Dependent on patient | LLTQ ADLs SMD=−1.36 LLTQ recreational activity SMD=−1.48 | Large Large |
| Bassett and Prapavessis14 (home exercise program) | Range of motion, stretching and strengthening exercises for the lower extremity | Not reported | Varied; dependent on ability to advance | Varied; average was 4.55 | Varied; dependent on patient recovery | Dependent on patient | LLTQ ADLs SMD=−0.96 LLTQ recreational activity SMD=−1.18 | Large Large |
| Bleakley et al.15 | Ankle range of motion, stretching and strengthening exercises | 30min | 1×/week (1 supervised, 4× HEP) | 20 | 4 weeks | 16 weeks | Karlsson score | Large |
| Cleland et al.38 | Mobility and strengthening exercises for the foot/ankle, resistive band and body weight exercises, balance and weight bearing functional activities | 30min | 1×/week supervised 1×/day HEP | 28 | 4 weeks | 6 months | LEFS SMD=2.61 FAAM ADLs SMD=1.92 NPRS SMD=−2.5 | Large Large Large |
| Ismail et al.16 (plyometric) | Bilateral and unilateral plyometric exercises including jumping, hopping and reaching in multi-directions | Not reported | 2×/week supervised | 12 | 6 weeks | 6 weeks | Climb down stairs (seconds) SMD=−1.99 Heel raise (times) SMD=4.86 Toe raise (times) SMD=3.67 Single leg stance (time) SMD=2.24 | Large Large Large Large |
| Ismail et al.16 (resistance) | Manual resisted exercise for ankle dorsiflexion, plantarflexion, inversion and eversion, active heel raises and toe raises, towel curl and marble pick-ups | Not reported | 2×/week supervised | 12 | 6 weeks | 6 weeks | Climb down stairs (seconds) SMD=−1.92 Heel raise (times) SMD=2.46 Toe raise (times) SMD=1.78 Single leg stance (time) SMD=1.28 | Large Large Large Large |
| Punt et al.17 | Wii FitTM for four balance games focusing on lateral weight shifting and multi-directional balance | 30min | 2×/week HEP | 12 | 6 weeks | 6 weeks | FAAM ADLs SMD=0.70 VAS during walking SMD=−0.75 VAS at rest SMD=−0.35 | Medium Medium Small |
| Heel pain | ||||||||
| Hyland et al.18 | Passive stretch to both gastrocnemius and soleus muscle, 3 repetitions with 30 second holds each | Not reported | 2× spread over one week supervised | 2 | 1 week | 1 week | VAS SMD=−2.26 PSFS SMD=−0.61 | Large Medium |
| Ryan et al.19 | Balance exercises, stretching and strengthening for ankle | Not reported | 1×/day HEP | 84 | 12 weeks | 12 weeks | FADI SMD=3.82 VAS with ADLs SMD=−6.47 | Large Large |
Abbreviations: ADLs, activities of daily living; FAAM, foot and ankle ability measure; FADI, Foot and Ankle Disability Index; HEP, home exercise program; LEFS, Lower Extremity Functional Scale; LLTQ, Lower Limb Tasks Questionnaire; NPRS, Numeric Pain Rating Scale; PSFS, Patient Specific Functional Scale; SMD, standardized mean difference; VAS, Visual Analog Scale; VISA, Victorian Institute of Sports Assessment.
Initial searches identified 444 studies for AT, 1039 for ankle sprains, and 563 for plantar heel pain. After title/abstract and full text screening, 13 were included and SMDs were calculated.6,8–19 Upon reaching out to primary authors for data necessary for SMD calculation, one study was added.38 Overall, there were 14 studies, with seven studies included for AT, five for ankle sprains, and two for plantar heel pain.6,8–19,38Fig. 1 outlines the search results.
Methodological quality assessmentThe Physiotherapy Evidence Database (PEDro) Scale was used to assess the quality of the included studies. The PEDro scale, comprised of 11 criteria and shown to be valid and reliable, is used to evaluate the external and internal validity of randomized controlled trials.39,40 The two reviewers agreed on published PEDro scores for the 14 studies.6,8–19,38
Methodological quality ratings were given to each of the studies via the PEDro scale, with a score of 7 or above considered to be ‘high’ quality, 5–6 was ‘fair’ quality, and 4 or below was ‘poor’ quality.41 The quality ratings are provided in Table 3. The mean score for AT was 7.29 (range 5–8), 7 (range 6–8) for the ankle sprain studies, and 5 (range 4–6) for the studies related to plantar heel pain, with AT and ankle sprains considered ‘high’ quality and plantar heel pain considered ‘fair’ quality. All of the studies met the criteria for random allocation, similar baseline characteristics between groups, between group statistical comparisons and point measures and measures of variability for at least one key outcome.6,8–19,38 None of the studies met the criteria for blinding of the subjects or treatment provider; however this is common in most physical therapy trials. Regardless, the lack of blinding in both these populations has not been shown to impact the overall magnitude of effect in clinical trials.42Fig. 2 provides the risk of bias across studies.
PEDro scores for included studies.
| Reference | Item* | Total score‡ | Study quality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1† | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
| Achilles tendinopathy | |||||||||||||
| Beyer et al.6 | Y | Y | N | Y | N | N | N | N | Y | Y | Y | 5 | Fair |
| Rompe et al.8 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Rompe et al.9 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Rompe et al.10 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Silbernagel et al.11 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Stevens and Tan12 | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 7 | High |
| Yu et al.13 | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 | High |
| Ankle sprain | |||||||||||||
| Bassett and Prapavessis14 | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 | Fair |
| Bleakley et al.15 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Cleland et al.38 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Ismail et al.16 | Y | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 | Fair |
| Punt et al.17 | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 7 | High |
| Heel pain | |||||||||||||
| Hyland et al.18 | Y | Y | N | Y | N | N | N | N | N | Y | Y | 4 | Poor |
| Ryan et al.19 | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6 | Fair |
Out of ten; Y=criterion satisfied and N=criterion not satisfied.
2, Subjects randomly allocated to groups.
3, Allocation was concealed.
4, Groups similar at baseline regarding most important prognostic indicators.
5, Blinding of subjects.
6, Blinding of all therapists.
7, Blinding of all assessors who measured at least one key outcome.
8, Measures of key outcomes were obtained from more than 85% of those initially allocated to groups.
9, All subjects for whom outcome measures were available received the treatment or control condition as allocated or where this was not the case, data was analyzed by “intention to treat”.
10, Results of between group statistical comparisons are reported for at least one key outcome.
11, Study provides both point measures and measures of variability for at least one key outcome.
Outcome measures varied across the included studies, which contributed to variations in overall effect size. Large and medium effects were observed in all of the studies for AT and plantar heel pain, and all but one of the studies related to ankle sprains.6,8–16,18,19,38,43 For AT, large effect sizes were observed in seven studies, with the VISA and visual analog scale (VAS) the most common outcome measures.6,8–13 Two studies had medium effects and used the VISA, VAS and Total Balance Index as outcome measures.12,13 For ankle sprains, large effect sizes were reported in four studies14–16,38 that used a variety of outcome measures. One study, Punt et al.,17 reported medium effect sizes for the VAS during walking and the Foot and Ankle Ability Measures of Daily Living subscale (FAAM ADL), and small effect sizes related to the VAS at rest. For the two studies investigating plantar heel pain,18,19 there were large effects using the VAS and Foot and Ankle Disability Index (FADI), whereas a medium effect was observed for the study using the patient specific functional scale (PSFS). Table 2 provides the SMDs for the studies.
Single session durationThe majority of the studies did not report the duration of time spent in a single session of exercise therapy. Of the seven studies investigating AT, five did not report single session duration.8–12 In the two studies that did report single session duration, the time was variable or 22min, depending on the exercise group in one study,6 and 50min per session in the other.13 Three of the four studies for ankle sprains reported session durations of 30min,15,17,38 and none of the studies for plantar heel pain provided single session duration.18,19
Frequency of interventionThe frequency of intervention varied across all studies. For AT, frequency ranged from once per day to three times per week, with twice a day, seven days a week being the most common.6,8–13 In six of the seven studies, patients were prescribed a HEP, and in only one study were patients supervised in the clinic.6,8–13 Frequency varied in one study for ankle sprains (where patients performed both supervised exercise and a HEP or only a HEP depending on the group they were in),14 or was two or five times per week (with different groups performing either supervised exercise or a HEP, or a combination of the two, depending on the study).15–17,38 For plantar heel pain, Hyland et al.18 prescribed a frequency of supervised exercise two times over one week, and Ryan et al.19 used a HEP frequency of once a day.
Total number of sessionsSimilar to frequency of intervention, the total number of sessions varied greatly. One hundred sixty eight (i.e., the number of sessions when exercising two times per day seven days per week) sessions was the most common dosing for AT (range 24–168),6,8–13 and 12 sessions (i.e., two times per week for 6 weeks; range 4.55–12) for ankle sprains.14–17 For the two studies related to plantar heel pain, one had two sessions18 and the other had 84 sessions.19
Duration of careFor AT, 12 weeks was the most common duration for receiving care, ranging from six weeks to six months.6,8–13 One of the studies for ankle sprains had a variable duration of care based on patient recovery, and the others ranged from one to six weeks.14–17 The duration of care for plantar heel pain was either one or twelve weeks.18,19
DiscussionThis review investigated the effects of exercise dose on outcomes in patients with AT, ankle sprains and plantar heel pain. Most of the included studies exhibited large effects regardless of exercise dose. Therefore, dosing parameters related to length and number of sessions, frequency, and duration of care may not be as important. Alternatively, there may be other factors (patient type, preference, adherence) that affect outcomes and confound the influence of exercise dose.
Nevertheless, the dosing variables that did not display large effects may be helpful in distinguishing less impactful exercise doses. They may provide insight for clinicians into which dosing variables should not be included in exercise prescription for patients with AT, ankle sprains and plantar heel pain. There was a small trend identified for patients with plantar heel pain. Hyland et al.18 treated patients with supervised visits only two times over a one week time frame, and found a medium effect on the PSFS. The patients treated in this fashion did, however, show a large effect size on the VAS. This is in contrast to Ryan and colleagues who showed that patients performing an exercise HEP one time per day had large effects related to both function and pain.19 This suggests that two supervised treatments over a week period may not have as large of an impact on function than a daily HEP would, but further investigation is warranted before making any definitive conclusions. Regardless, the number of studies on plantar heel pain was limited to two, and the overall dose varied widely, so this trend could have changed if a larger number of studies were included for analysis. These findings should be validated in prospective trials before recommendations can be made about these particular doses, but this finding shows promise that treatment frequency and overall number of sessions may influence outcomes in patients with plantar heel pain.
For ankle sprain, a HEP of two times per week was associated with small and medium effect sizes for patients,13 compared to large effect sizes for patients who received supervised exercise sessions two times per week.16 Compliance was not monitored in patients performing the HEP and this may have impacted the overall outcomes.13 Thus, this was not identified as a trend related to exercise dose and ankle sprains. It would be informative if future studies compared exercise only in a supervised setting versus a HEP with monitored compliance.
Interestingly, one other observation was seen in relation to specific sets and repetitions of exercise. In AT, Stevens and Tan12 found large and medium effects on the VISA and VAS with a similar exercise prescription for both groups. The only variable that was different was how patients participated in the exercise, where the group with medium effects performed a specific amount of sets and repetitions, and those with large effects performed a number of repetitions they could tolerate.12 One other study on AT was also associated with medium effects.13 However, it used a different outcome measure that may not have measured the same construct.12,13 Because of this, a study that uses the same outcome measures may provide a more accurate assessment of the magnitude of effect. These results need further validation.
Other influences on exercise prescriptionConfounding factors, such as stage of healing, psychosocial issues, compliance or ability to perform in an exercise program, and home and work demands, may alter the patient's exercise compliance. Unfortunately, these factors are not often taken into account during clinical trials.44 Along with a lack of measuring factors that confound compliance, the description of exercise interventions is for the most part poorly reported in clinical trials. As a result, attempts to duplicate specific dosing in the clinic may prove futile.45 Having valid dosing information, however, better informs clinical practice. It also allows for modification of dosing in future trials, to understand which variables are best.
There is evidence for a dose–response relationship between exercise and health outcomes, where various amounts of exercise provide either a benefit or a risk for overall health.25 However, it is unclear the specific dose necessary for different genders or ages for benefits.25,46 For general physical fitness, it is recommended individuals perform 75min of vigorous or 150min of moderate intensity exercise per week.25 Is it possible that for patients with AT, ankle sprains, or plantar heel pain there is an ideal of total exercise time they should perform to achieve optimal outcomes? If there is, should it be performed for the same amount of time each session, over the same frequency and duration of care? Another question is whether or not the exercise should be supervised or independent. As shown in this review, the studies varied in whether they used supervised sessions or a HEP.6,8–19,38 Lastly, clinicians and clinical trials often apply the principle of one size fits all with exercise, and rarely is it appropriate.32 That may also impact outcomes because even if compliance is monitored, it is not always clear if patients are performing exercise appropriately. Each of these suggestions adds to the complexities of dose, and shows that many factors influence patient outcomes.
LimitationsThere are several limitations to this review. First, the heterogeneity of outcome measures for pain and function makes comparison between studies challenging. Because of this, we included any outcome measure related to pain and function, which ultimately means the effect size on one outcome measure may not equal the effect size on a different outcome measure. Second, eleven studies used a HEP, but only four of these measured compliance.6,14,15,19 It is possible that if all studies utilizing a HEP had reported their compliance levels, results may have been different. Third, the overall methodological quality of the studies related to plantar heel pain was ‘fair,’ and this should be taken into account with the recommendation. Lastly, there were a limited number of studies for these disorders that focused on exercise therapy alone. Many others were not included because they used exercise therapy in conjunction with manual therapy, modalities, or other interventions. Because there were a limited number of studies meeting the inclusion criteria, further research is needed to help validate these findings.
ConclusionsSpecific exercise dosing variables to maximize outcomes for patients with AT, ankle sprains or plantar heel pain are lacking. The majority of studies included in this review showed large effect sizes, suggesting that session duration, number and frequency of sessions, and overall duration of care may be less important than other variables. One small trend related to exercise doses for patients with plantar heel pain was found, where a frequency of two visits over one week with a one week duration of care was related to a medium effect size in function. This was based off of only two studies, so further validation is necessary. Lastly, another trend was seen in patients with AT who were allowed to perform eccentric exercise sets and repetitions as tolerated and had large effect sizes, compared to patients prescribed a specific number of sets and repetitions who had only medium effect sizes. Because there is a plethora of factors involved with the effectiveness of exercise prescription, it is difficult to determine if these particular variables alone are responsible for the results. Continued research is necessary to determine the impact these variables may have on musculoskeletal disorders of the foot and ankle.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.