Although evidence-based practice has been widely used by physical therapists, data variation suggests that its implementation may be influenced by a number of factors. Population-specific information is required to help enhance the use of research in clinical practice.
ObjectiveTo identify the personal and organizational characteristics associated with the use of evidence-based practice by physical therapists providing services to people with stroke in Brazil.
MethodsA cross-sectional mail survey was conducted. The Brazilian versions of the questionnaires “Practitioner and Organizational Barriers to Evidence-based Stroke Rehabilitation” and “Evidence-based practice self-efficacy scale” were mailed to physical therapists. Logistic regression analysis was used to explore associations between personal and organizational characteristics with education, attitudes, beliefs, interest, and perceived role, perceived support, and organizational resources for evidence-based practice.
ResultsThe response rate was 36% (n=94). Ten characteristics explained 57% of the variance associated with attitudes and beliefs, and interest and perceived role for evidence-based practice. Nine characteristics explained 50% of the variance associated with perceived support and organizational resources for evidence-based practice. The most frequently cited barrier was lack of time (62%).
ConclusionsAlthough participants had positive attitudes regarding evidence-based practice, there is a need to develop a supportive organizational infrastructure, in addition to enhancing skills of the evidence-based practitioner, to increase research integration in physical therapy practice for assessing and treating people with stroke. Potential strategies should include use of evidence-based practice during undergraduate programs, partnership with professional practice-oriented organizations, and investments to enable research-related activities.
Evidence-based practice (EBP) is a five-step process, in which clinical decisions are based upon high-quality clinical research, taking into account the wishes, expectations, and values of the client, as well as the therapist's experiences and knowledge.1–3 Growing evidence indicates that an evidence-based approach is associated with improvements in clinical outcomes of people with stroke and widespread benefits, which include client's improved satisfaction and cost reductions for the health care system.4–6 However, successful implementation of EBP is a dynamic process, which is influenced not only by the characteristics of the physical therapists, but also by organizational factors related to the workplace setting and administrative support.7
A systematic review8 examined 12 cross-sectional studies that investigated EBP knowledge, skills, behavior, opinion, and barriers in physical therapy. Although the majority of the respondents have positive opinions related to EBP, data regarding knowledge, skills, and barriers varied considerably among the studies, preventing definite conclusions. Overall, difficulties for implementing EBP were mostly related to lack of knowledge and skills (8%–84%), lack of support from employers (6%–56%), and lack of time (31%–94%).8 More recent studies, which have tried to identify barriers to EBP among physical therapists in Austria,9 Brazil,3 Colombia,10 Iceland,11 and Saudi Arabia,12 also reported imprecise results. These variations suggest that barriers to EBP may be influenced by differences in entry-level training, health care systems, and professional practice across the countries, and more specific information is required before drawing conclusions. Implementation of EBP, for example, could also be population-specific, as it depends on availability of high-quality clinical research. A simple search on the PEDro website (www.pedro.org.au) revealed considerable differences regarding the number of available systematic reviews and clinical trials among the subareas of physical therapy, e.g., Neurology (5000 studies) and Ergonomics (800 studies). Differences are also observed within subareas, considering different populations, e.g., Stroke (2500 studies) and Spinal Cord Injury (300 studies). To narrow the gap between knowledge and practice, the identification of factors that exert the greatest influence on preventing the implementation of EBP to a specific population is, therefore, reasonable.
Specific personal and organizational barriers to EBP of physical therapists providing service to people with stroke have already been examined in Canada,13 suggesting that, although current university programs have been emphasizing the foundations of skills to implement EBP, organizational barriers, such as lack of protected time to search and appraise the research evidence may still continue to prevent its implementation. However, this study was published 10 years ago and may not reflect the current personal and organizational barriers to EBP of physical therapists, who provide services for people with stroke in Brazil. Furthermore, recent data have demonstrated that although physical therapists, who provide service to people with stroke, recognize EBP as a framework for improving the quality of care, they do not employ research-based evidence to its fullest extent.14
Therefore, the primary aim of this study was to identify the personal and organizational characteristics associated with the implementation of EBP by physical therapists providing services to people who had suffered a stroke in Brazil. The specific research questions were:
- 1.
What is the percentage of physical therapists, who agree or disagree with statements related to education, attitudes and beliefs, and interest and perceived role in EBP delivered to people with stroke?
- 2.
What are the personal and organizational characteristics associated with education, attitudes and beliefs, and interest and perceived role for EBP?
- 3.
What are the personal and organizational characteristics associated with perceived support and organizational resources for EBP?
- 4.
What are the self-efficacy ratings for implementing EBP and which characteristics are associated with self-efficacy?
- 5.
What are the perceived barriers to EBP?
A mail survey with physical therapists providing services to people with stroke in Brazil was conducted. Two strategies were used to recruit the maximum number of physical therapists possible. The first strategy was the modified Dillman three-step mailing procedure,15 which consisted of a first mailing of the questionnaire, followed by a postcard thank-you/reminder and a second mailing of the questionnaire to the non-respondents. The second strategy was the publication of the questionnaire on the website of a professional practice-oriented organization (Associação Brasileira de Fisioterapia Neurofuncional – ABRAFIN) focused on physical therapists who provide services to people with neurological conditions.
This study was approved by the ethical review board of the Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil (CAAE-34540014200005149) and followed previous recommendations from Salbach et al.13 Consent was considered implied for physical therapists who answered the questionnaires.
Participants and samplingPhysical therapists were considered eligible for the study if they: (1) were currently practicing and providing services to adults with stroke; (2) entered the Survey Monkey website through a provided link for research purposes and questionnaires. Potential participants were recruited through electronic addresses from a professional practice-oriented organization (e.g. ABRAFIN), which also published the survey link on its website, in order to increase visibility of the study. The questionnaires were sent via e-mail through the link produced at the SurveyMonkey website (https://en.surveymonkey.com/user/sign-in/ [s.d.]). The final sample was comprised of physical therapists who answered the questionnaires and reported providing services to people who had suffered a stroke. Eligible individuals, who returned the questionnaires with all items unanswered, were considered as refusals.
Questionnaires – “Practitioner and Organizational Barriers to Evidence-based Stroke Rehabilitation” and “Evidence-based practice self-efficacy scale”The Brazilian versions of the questionnaires “Practitioner and Organizational Barriers to Evidence-based Stroke Rehabilitation” and the “evidence-based practice self-efficacy scale” were mailed to all physical therapists.13,16 The cross-cultural adaptation of the questionnaires were previously conducted and followed recommended procedures.17–19
The questionnaire items were designed to identify practitioner and organizational factors that influence EBP. Sub-groups of items were used to evaluate education (three items), attitudes and beliefs (seven items), interest (two items) and perceived role (three items), self-efficacy to perform EBP activities (two items), perceived organizational and peer support (two items), and organizational resources and support (six items). One item was used to identify the most frequent barriers to updating clinical practice with new knowledge. Items were added to the end of the questionnaire, to evaluate respondent demographics, practice characteristics, and work settings. For the majority of the items, respondents indicated their level of agreement on a 5-point Likert scale. Response options for items related to the presence of organizational resources were “yes,” “no,” and “do not know”.13 Detailed information regarding the questionnaires or the full versions can be obtained from the authors upon request.
After accessing the email, participants were requested to enter the Survey Monkey website through the provided link. On the first page, they were asked to read and sign the consent form. If they agreed to participate, they were immediately directed to the questionnaires, and could answer as many questions as they wanted.
Data analysesDescriptive statistics was provided to report the respondents’ and practice characteristics. The prevalence of practitioner and organizational factors was estimated using percentages. To answer question 1, i.e., percentage of physical therapists, who agree/disagree with statements related to EBP, the categories were combined, following previous recommendations.8 For the statements with positive responses, i.e., “strongly agree” and “agree” categories were combined into “agree” category, and the “neutral”, “disagree” and “strongly disagree” categories were combined into “disagree” category. For the statements with a negative response, the “strongly disagree” and “disagree” categories were combined to form a “disagree” category, and the “strongly agree”, “agree” and “neutral” categories were combined to form an “agree” category. For items with “yes”, “no”, and “do not know” response categories, the latter two categories were combined, based on the assumption that the effect of not knowing about the presence of a resource would have a similar effect as not having the resource.13
To answer question 2, i.e., characteristics associated education, attitudes and beliefs, and interest and perceived role regarding EBP, a binary logistic regression analysis was used to examine the relationships between socio-demographic and practice characteristics of the respondents (independent variables) and their responses regarding EBP (dependent variable). All independent variables were combined into categories, in order to produce nominal data, as previously described. The responses of each participant were combined as “positive” or “negative”, producing a dichotomous dependent variable. Analysis was conducted including only the independent variables that were significantly correlated (α<0.05). Given the exploratory nature of the analysis, statistics were calculated without adjustment for confounding.
To answer question 3, i.e., characteristics associated with perceived support and organizational resources, a binary logistic regression analysis was used to examine the relationships between organizational characteristics (independent variables) and responses related to perceived support and organizational resources for EBP (dependent variable). The analysis followed the same steps previously described.
To answer question 4, i.e., self-efficacy ratings and associated characteristics, descriptive statistics (i.e., mean, SD, and range) were reported, followed by logistic regression analysis to examine the relationships between personal and organizational characteristics, and self-efficacy. The median self-efficacy rating (≤76 points/>76 points) was used as cut-off point for dichotomizing the respondents.13
To answer question 5, i.e., perceived barriers to EBP, the percentage of respondents of each indicated barrier was provided.
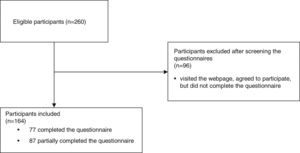
ResultsFlow of questionnaires, respondents’ characteristics, availability of resources, and support to promote evidence-based practiceThe questionnaires were mailed to the physical therapists between December 2015 and June 2016. Of the 260 individuals who were eligible 96 (37%) visited the webpage, agreed to participate, but did not answer the questions. The response rate from the collected data was 63% (164/260 individuals). However, only 77 individuals (30%) answered all questions and 87 (33%) partially completed the questionnaires. The response rate for most analyses was 36% (94/260 individuals). Fig. 1 illustrates the flow of participants over the course of the study.
Table 1 provides the respondents’ practice characteristics and the characteristics of their work setting. Respondents were aged between 20 and 60 years old (mean: 32 years, SD: 7), and 75% were women. A bachelor's degree followed by additional certificate degree specialization was the most commonly cited highest degree (52%), and 78% of the respondents reported having less than 10 years of clinical practice experience. The majority of the respondents worked more than 20h/week (94%), providing services to five to 10 patients per week (50%), of whom two to five were patients who had suffered a stroke (67%). The most frequently cited characteristics of working settings were urban locations (94%) and employment in a private long-term care facility (47%). Participants from the five regions of Brazil were included: southeast (52%), south (15%), northeast (15%), midwest (12%) and north (6%).
Characteristics of the respondents, their practice, and practice settings (n=164) in a study investigating characteristics associated with evidence-based practice.
| Characteristic | n | % |
|---|---|---|
| Age (y) | 164 | |
| 20–29 | 63 | 39 |
| 30–39 | 79 | 48 |
| 40–49 | 16 | 10 |
| 50+ | 6 | 3 |
| Sex | 162 | |
| Men | 40 | 25 |
| Women | 122 | 75 |
| Bachelors’ degree (y) | 96 | |
| ≤1998 | 8 | 8 |
| >1998 | 88 | 92 |
| Highest degree | 164 | |
| Bachelor's | 43 | 26 |
| Specialization | 86 | 52 |
| Master's | 21 | 13 |
| Ph.D. | 14 | 9 |
| Years practiced | 162 | |
| <5 | 65 | 40 |
| 5–10 | 61 | 38 |
| 11–15 | 21 | 13 |
| >15 | 15 | 9 |
| Member of professional organization | 93 | |
| Yes | 32 | 35 |
| No | 61 | 65 |
| Hours of work per week | 94 | |
| <20 | 6 | 6 |
| 20–30 | 29 | 31 |
| 31–40 | 29 | 31 |
| >40 | 30 | 32 |
| Number of patients assisted per day | 92 | |
| <5 | 12 | 13 |
| 5–10 | 45 | 49 |
| 11–15 | 18 | 20 |
| >15 | 17 | 18 |
| Number of stroke patients assisted per day | 93 | |
| <2 | 20 | 21 |
| 2–5 | 62 | 67 |
| 6–10 | 8 | 9 |
| >10 | 3 | 3 |
| Member of multidisciplinary team | 94 | |
| Yes | 60 | 64 |
| No | 34 | 36 |
| Clinical instructor | 160 | |
| Yes | 35 | 22 |
| No | 125 | 78 |
| Participation in research activities | 162 | |
| Yes | 65 | 40 |
| No | 97 | 60 |
| Location | 161 | |
| Urban | 152 | 94 |
| Suburban | 6 | 4 |
| Rural | 3 | 2 |
| Type of facility | 158 | |
| Hospital | 24 | 15 |
| Rehabilitation hospital | 12 | 8 |
| Private long-term care facility | 74 | 47 |
| Public long term care facility | 19 | 12 |
| Community care access center | 6 | 4 |
| University/educational institution | 23 | 14 |
| Number of physical therapists at facility | 90 | |
| ≤5 | 60 | 67 |
| 6–15 | 21 | 23 |
| >15 | 9 | 10 |
| Number of neurological physical therapists at facility | 90 | |
| ≤5 | 70 | 77 |
| 6–15 | 19 | 21 |
| >15 | 2 | 2 |
| Teaching institution | 93 | |
| Yes | 28 | 30 |
| No | 65 | 70 |
Regarding the availability of resources and support to promote EBP, the majority of the respondents had access to relevant databases and Internet at their facilities (54%) or at home/other locations (89%). On the other hand, the majority of the respondents did not have access to scientific journals in paper form at their facilities (72%) or to a mentor to assist with EBP (79%), and worked at a facility that did not mandate the use of current evidence in practice (90%), did not provide protected time for literature review and appraisal (85%), and did not provide financial support to educational meetings and conferences (82%). Half of the respondents stated that the use of current research in clinical practice was supported in their working environment. Detailed information is provided in Table 2.
Availability of resources and support to promote evidence-based practice (EBP) (n=94).
| Item | n | Response (%) | ||
|---|---|---|---|---|
| Yes | No | Do not know | ||
| I have access in my facility to current research through professional journals in their paper form | 94 | 26 | 72 | 2 |
| I have the ability to access relevant databases and the Internet at my facility | 94 | 54 | 45 | 1 |
| I have the ability to access relevant databases and the Internet at home or locations other than my facility | 94 | 89 | 10 | 1 |
| A resource person is available at my facility to assist me with EBP | 94 | 17 | 79 | 4 |
| My facility mandates the use of current research findings in practice | 94 | 8 | 90 | 2 |
| My facility provides protected time to conduct literature reviews and appraise the literature | 93 | 15 | 85 | 0 |
| My facility provides financial support to attend educational meetings and conferences | 94 | 18 | 82 | 0 |
Although most of the respondents received formal training on EBP (60%) and believed that it helped clinical practice (92%), the majority needed to increase the use of evidence (83%) and/or to improve their skills to incorporate evidence into their daily practice (94%). In addition, the majority of the respondents were aware of their responsibilities in conducting literature reviews (62%), evaluating the quality of the literature (90%), and interpreting whether research findings applied to their patients (89%), and did not believe that EBP placed unreasonable demands on physical therapists’ lives (40%). Most of the respondents (44%) agreed that there was a definite gap between research and clinical practice. Detailed information is provided in Table 3.
Education, attitudes and beliefs, and interest and perceived role in evidence-based practice (EBP) (n=98).
| Item | n | Response (%) | ||
|---|---|---|---|---|
| Disagree | Neutral | Agree | ||
| Education | ||||
| I learned the foundations for EBP as part of my academic preparation | 95 | 32 | 9 | 59 |
| I received formal training in search strategies for finding research relevant to my practice | 95 | 30 | 7 | 63 |
| I received formal training in how to critically evaluate research literature as part of my academic preparation | 94 | 31 | 11 | 58 |
| Attitudes/Beliefs | ||||
| Application of EBP is necessary in the practice of physical therapy | 97 | 1 | 10 | 89 |
| Literature and research findings are useful in my day-to-day practice | 98 | 1 | 5 | 94 |
| The adoption of EBP places an unreasonable demand on physical therapists | 96 | 40 | 33 | 27 |
| EBP improves the quality of patient care | 96 | 0 | 10 | 90 |
| EBP helps me make decisions about patient care | 95 | 1 | 5 | 94 |
| EBP does not take into account patient preferences | 95 | 53 | 22 | 25 |
| There is a definite divide between research and practice | 96 | 35 | 21 | 44 |
| Interest/Perceived role | ||||
| I need to increase the use of evidence in my daily practice | 97 | 5 | 12 | 83 |
| I am interested in learning or improving the skills necessary to incorporate EBP into my practice | 96 | 1 | 5 | 94 |
| Physical therapists should be responsible for conducting their own literature reviews to answer their clinical questions | 95 | 23 | 15 | 62 |
| Physical therapists should be responsible for critically evaluating the quality of the literature to address their clinical questions | 95 | 4 | 6 | 90 |
| Physical therapists should be responsible for interpreting whether research findings apply to their individual patients | 95 | 3 | 8 | 89 |
There were no personal or organizational characteristics significantly associated with education on EBP. Six characteristics (i.e., sex, participation in research, work in a multidisciplinary team, access to scientific journals, number of treated patients per day, and number of full-time physical therapists at the facilities) were significantly associated with attitudes and beliefs, and four characteristics (i.e., being member of a professional practice-oriented organization, hours of work per week, having access to databases and internet at work, and having facility support for access to current research findings) were significantly associated with interest and perceived role on EBP. Logistic regression indicated that those characteristics could explain 57% of the variance associated with attitudes and beliefs, and interest and perceived role for EBP (X2=17.0, p=0.04, Nagelkerke R2=0.57).
Personal and organizational characteristics associated with perceived support and organizational resources for evidence-based practiceNine characteristics (i.e., sex, belonging to a professional practice-oriented organization, participation in research, supervising physical therapy students, working at a teaching institution, working at a facility involved in stroke research, working in a multidisciplinary neurorehabilitation team, years of experience with stroke clientele, and number of patients per day) were associated with perceived support and organizational resources for EBP. Logistic regression indicated that those characteristics could explain 50% of the variance associated with perceived support and organizational resources for EBP (X2=34.9, p<0.01, Nagelkerke R2=0.50).
Self-efficacy ratings and associated characteristicsSelf-efficacy ratings for 12 activities or skills necessary to implement EBP were investigated. Average ratings were greater than 80% for identifying a clinical problem following a patient assessment (83%), formulating a question to guide a literature search (81%), understanding patients’ needs and treatment preferences (88%), deciding on an appropriate course of action in collaboration with the patient (89%), and continually evaluating the effect of practice (81%). Average ratings were between 50% and 80% for effectively searching the relevant literature (78%), interpreting results of statistical tests, such as t tests and chi-square (51%), applying evidence from literature to the individual patient (74%), and critically appraising the literature for reliability and relevance (72%), the measurement properties of outcome measures (60%) and the strengths and weaknesses of different study designs (62%). Average ratings below 50% were observed only for interpreting results of statistical analyses, such as linear or logistic regression (43%). Detailed information is provided in Table 4.
Self-efficacy to perform evidence-based practice activities (n=94).
| Activity | n | Score (/100%) | ||
|---|---|---|---|---|
| Mean | SD | Range | ||
| Identify clinical problems following a patient assessment | 94 | 83 | 13 | 40–100 |
| Formulate a question based on the clinical problem to guide a literature search | 94 | 81 | 20 | 10–100 |
| Effectively search the relevant literature to address the question | 94 | 78 | 21 | 10–100 |
| Critically appraise the literature for reliability and relevance | 94 | 72 | 21 | 0–100 |
| Critically appraise the psychometric properties of outcome measures | 94 | 60 | 26 | 10–100 |
| Critically appraise the strengths and weaknesses of different study designs | 94 | 62 | 27 | 0–100 |
| Interpret results of statistical procedures such as t tests and chi-square tests | 93 | 51 | 29 | 50–100 |
| Interpret results of statistical procedures such as linear or logistic regression | 93 | 43 | 29 | 0–100 |
| Appropriately apply evidence from the literature to the individual patient | 93 | 74 | 22 | 0–100 |
| Understand your patient's needs and treatment preferences | 93 | 88 | 12 | 50–100 |
| Decide on an appropriate course of action in collaboration with the patient | 94 | 89 | 12 | 50–100 |
| Continually evaluate the effect of your practice | 94 | 81 | 25 | 10–100 |
Regression analysis indicated that the highest degree and years of experience with stroke clientele were associated with EBP self-efficacy (n=92). The odds of rating the self-efficacy above 76% were 11.2 (95% CI 2.2, 20.1) if physical therapists had a master's or doctoral degree. In addition, the odds of rating the self-efficacy above 76% were higher among physical therapists with more than five years of experience with stroke clientele, e.g., 5–10 years (OR: 2.9; 95% CI 1.1, 4.6).
Self-reported barriers to evidence-based practiceThe four mostly frequently cited barriers were insufficient time provided by management (62%), lack of generalizability of research findings to the patient population (33%), lack of understanding of statistical analyses (32%), and lack of support among colleagues (32%). The only barrier cited by fewer than 10% of the respondents was lack of interest (5%).
DiscussionThis study aimed at identifying the personal and organizational characteristics associated with the implementation of EBP by physical therapists providing services to people who had suffered a stroke, in Brazil. The results indicated that nine organizational characteristics were significantly associated with attitudes and beliefs, and interest and perceived role of EBP; and eight organizational characteristics were significantly associated with perceived support and organizational resources. Personal characteristics showed little association with education, attitudes, beliefs, interest, or perceived role and support for EBP. Physical therapists somehow involved with research/teaching were more likely to be engaged in implementation of EBP and lack of protected time for literature review and critical appraisal was the most self-reported barrier.
A common personal barrier to the implementation of EBP was lack of education regarding the foundations for EBP as part of academic preparation.20 However, a higher proportion of Brazilian respondents (59%) reported having formal education on the principles of EBP compared to Canadian (45%) and Austrian (42%) physical therapists, who participated in similar studies.9,13 On the other hand, the majority of the Brazilian physical therapists indicated the need to increase the use of evidence in their daily practice (83%) and to learn/improve skills to incorporate EPB into clinical practice (94%). These results suggest that although dissemination of information has increased, the implementation of EPB still remains ineffective. If the final goal is to speed the rate of adopting EBP by physical therapists, funding agencies for research need to direct more attention toward the development of strategies of active implementation, where knowledge is translated into practice.21
Contrary to previous studies,13,22 the results demonstrated that, in Brazil, personal characteristics were poorly associated with education, attitudes, beliefs, interest, and perceived role and support for EBP. However, self-efficacy ratings were considerably low for effectively understanding and critically appraising the research literature (65%), particularly with respect to understanding statistical procedures (47%), which was similar to previous studies.9,12,13,22 Physical therapists, who have low self-efficacy for understanding and critically appraising the research literature and translating it into clinical practice, were less likely to perform these activities than people who perceived their level of skill to be higher.13 Strategies to facilitate physical therapists’ access to and appraisal of the research literature should be implemented by journals and researchers, such as use of non-technical language, glossaries of research terms, and quality ratings of studies.23
On the other hand, many organizational characteristics were associated with EBP, such as lack of access of scientific journals in their paper form (72%), protected time for literature appraisal (85%), financial support (82%), and EBP mentoring (79%). In addition, organizational characteristics were significantly associated with education, attitudes, beliefs, interest, and the perceived role of and support for EBP. These results suggested that the influence of the personal characteristics may be underestimated, when there was limited organizational support for implementing EBP. In other words, the findings do not mean that personal characteristics were not important, but they seemed to be covered if physical therapists were not provided with time, material and administrational support to obtain and comprehend the evidence before converting it into clinical practice. Interestingly, the majority of the identified organizational items could be abridged in the umbrella of research participation. This finding is of concern, since most of the respondents did not participate in any research activity (60%) and might not be interested in the academic environment. In addition, a high percentage of the participants (44%) believed there was a definite divide between research and clinical practice. Previous studies suggested that organizational strategies implemented at the workplace level, such as leadership support, EBP mentors, provision of resources such as time and money, and dissemination of information (e.g., workgroups and journal clubs) should be implemented to bridge the gap between research and clinical practice.24,25 Those strategies have the potential to reduce the enormous amount of existing scientific knowledge that remains unused in clinical practice,26 but the evidence underpinning their success in the area of rehabilitation is limited. In addition to those strategies, the results of this study suggest that implementation of EBP in neurological rehabilitation should be initiated at the undergraduate level and could be further optimized with the support of professional practice-oriented organizations, such as ABRAFIN. Foundations for EBP should be part of the academic preparation and therapeutic interventions discussed in applied disciplines at undergraduate programs should be those with proven clinical efficacy. During the educational clinical internship, the students should be provided with appropriate mentoring and time for searching and appraising the literature, and any clinical practice without reasonable evidence should be excluded. Daily checklists containing EBP steps, such as creating a clinical question, searching for evidence, and appraising the quality of the evidence, should be included in the clinical internships. In addition, professional practice-oriented organizations (e.g., ABRAFIN) should develop strategies to encourage EBP, as the majority of the included participants were associated to these organizations. Strategies could include such things as educational meetings and conferences, dissemination of information (e.g., email, websites), synthesis of evidence, support for developing structured environments for EBP.
Amongst the self-reported barriers, the insufficient time provided by management was by far the most cited by the respondents (62%). The results were in accordance with those reported by a previous systematic review, which indicated that lack of time was the most cited barrier by physical therapists (ranging from 31 to 94%).8 Without protected time to conduct literature searches and critically appraise the evidence, physical therapists cannot take advantage of organizational facilitators that might be present in the workplace. A survey conducted with a random sample of Brazilian physical therapists indicated that additional barriers besides lack of time (61%) may prevent EBP implementation in Brazil, such as difficult in obtaining full-text papers (80%) and language of publication of scientific papers (70%).3 As those barriers were not originally described in the list of options, the respondents of the present study might not have considered including them in the box of additional answers.
This study had some limitations. Although efforts were made to access all Brazilian physical therapists, who provide services to people who had suffered a stroke, the sample was not randomly selected and may not, therefore, be fully representative of the population of interest. Moreover, half of the respondents partially completed the questionnaire, which might be related to the length of the questionnaires and lack of time or interest. Respondents who completed the questionnaires were likely to be individuals with some interest in EBP, which may have led to an overestimation of the percentage of physical therapists with knowledge and positive attitudes toward EBP implementation. Unfortunately, as the response rate for most analyses was 36%, the sample may not be fully representative of the population of Brazilian physical therapists, who provide service to people who had suffered a stroke. In addition, the sample was comprised of Brazilian physical therapists working in predominantly urban locations; it was, therefore, unclear whether and to what extent the results reflected research-evidence uptake in suburban or rural areas. Lastly, although self-reported surveys are the most valid methods to assess beliefs, attitudes and opinions,27 there are potential biases inherent to the study design that should be taken into consideration, such as acquiescent response styles, social desirability, negative affectivity bias, and extreme response styles.12,28
ConclusionBrazilian physical therapists, who provide services to people who had suffered a stroke, have positive attitudes and beliefs regarding EBP, as well as interest to improve skills and to increase the use of evidence in their daily practice. Overall, there is a need to develop a supportive organizational infrastructure, in addition to enhancing skills of the evidence-based practitioner to increase research integration in physical therapy practice for treating people with stroke. Potential strategies should include: EBP mentoring, provision of resources, such as time and money, and investments in research-related activities.
Conflicts of interestThe authors declare no conflicts of interest.
Brazilian Government Funding Agencies (CNPq and FAPEMIG).