Studies with functional and applicable methods and new cognitive demands involving executive function are needed to improve screening, prevention and rehabilitation of cognitive impairment and falls.
Objectiveto identify differences in gait, dual task performances, and history of falls between elderly people with preserved cognition, mild cognitive impairment and mild Alzheimer's disease.
MethodA cross-sectional study was conducted. The sample consisted of 40 community-dwelling older adults with preserved cognition, 40 older adults with mild cognitive impairment, and 38 older adults with mild Alzheimer's disease. The assessment consisted of anamneses, gait (measured by the 10-meter walk test), dual task (measured by the Timed Up and Go Test associated with the motor-cognitive task of calling a phone number), and history of falls in the past year.
ResultsThere were no differences among all groups for all variables. However, the Alzheimer's disease Group performed significantly worse in the dual task than the other groups. No item of dual task could distinguish people with preserved cognition from those with mild cognitive impairment. The groups with cognitive impairment included more fallers, and specific characteristics in history of falls between groups were identified.
ConclusionDual task could distinguish Alzheimer's disease patients specifically from other cognitive profiles.
Cognitive impairment, including Alzheimer's disease (AD) and mild cognitive impairment (MCI) exerts an enormous impact on global society and it is one of the leading causes of disability and dependence.1 Cognitive decline is the primary clinical marker of MCI and dementia, but some studies have reported motor deficits in gait and dual task situations in mild stages of cognitive impairment.2,3
A temporal disruption of gait is observed in people with AD.4,5 Altered frontal cognitive capacities, primarily executive function (also called control of cognitive processes), reduce the allocation of attentional resources in the brain, which compromises postural stability and gait and increases the risk of falls.4 Some studies have used gait associated with a cognitive task to distinguish elderly people with different cognitive profiles.2,3,6 However, these studies were restricted to cognitive tasks involving verbal fluency or calculations,2,3,6 which do not reflect a common, complex and challenging executive function task. Also, few studies compared mobility performance between the elderly with preserved cognition (PC), MCI and AD, but the AD samples in these studies were not restricted to a specific phase of the disease.3,6
It is known that MCI, unlike dementia, may be reversed to normal or at least delayed by using proper treatment strategies.1 Dementia, falls and age-related health conditions are major public health problems. Therefore, the identification of clinical tests that can differentiate the three populations: PC, MCI, and mild AD, with new functional and applicable cognitive demands involving executive function, are needed to improve screening, prevention and rehabilitation.
The purpose of this study was to identify differences in gait and dual task performances and history of falls between elderly subjects with PC, MCI and mild AD. It was hypothesized that the dual task test could primarily differentiate the three groups, and there would be more falls in the elderly with cognitive impairment.
MethodParticipantsThe Universidade Federal de São Carlos (UFSCar) ethics research committee (São Carlos, SP, Brazil) approved the study (819.668/2014), and all participants signed an informed consent form.
Potential participants included community-dwelling older adults aged 65 years and older who could be contacted by phone or at home. Participants were recruited from health centers/units, the School Health Unit of UFSCar, and the Open University for older adults (São Carlos, SP, Brazil). Inclusion criteria were the ability to walk at least 10 meters alone without a walking aid, the availability to participate in the proposed assessments, and admission into one of the three elderly groups studied. Exclusion criteria were the presence of motor alterations after stroke, neurological disorders that interfered in cognition or mobility, severe uncorrected visual or auditory disorders, and advanced or moderate AD.
An experienced neurology professor confirmed the diagnosis of MCI, AD (mild stage) or PC. Subjects were divided into three groups based on their cognitive profile. Elderly subjects with a normal Mini-Mental State Examination (MMSE) score for Brazilian elderly population (MMSE score of 20 points for illiterates; 25 for 1–4 years of education; 26.5 for 5–8 years; 28 for 9–11 years and 29 for higher levels of education),7 and who did not exhibit criteria for MCI or dementia were considered PC.
The following criteria were used for MCI: (1) cognitive complaint, reported by the subjects or an informant or caregiver (a person who stayed with the subject at least half a day, four days per week); (2) objective cognitive impairment not related to delirium, with a score of 0.5 on the Clinical Dementia Rating Scale (CDR)8; normal global cognitive function for educational level, as assessed by the MMSE7; (4) preserved function, as assessed using the Pfeffer Scale9; and (5) absence of clinical dementia.10,11
The diagnosis of AD used the Diagnosis and Statistical Manual of Mental Disorders (DSM-V TR).10 Only elderly people with CDR=1 were included in this group.
Testing procedure and fallsThe subjects were instructed to wear comfortable clothing and their usual closed shoes, to have eaten at least 1h prior to the tests, to have avoided vigorous exercise the day before the tests, and to bring any necessary visual or auditory aids before the assessment. Two trained professionals assessed the subjects. The tests were applied in a closed environment that was as free from visual and auditory stimuli as possible.
Descriptive variables were assessed using a questionnaire (with the help of caregiver if necessary), categorized by age, gender, time of diagnosis for the AD Group, body mass index, educational level, abdominal circumference, use of multi/bifocal glasses, and use of walking aids. The Geriatric Depression Scale (GDS)12 and Minnesota Questionnaire were used to assess depression and levels of physical activity, respectively.13,14 GDS is commonly used in clinical practice to screen for risk of depression in an elderly population. In its short version, the total score is 15 points and 5-point or more indicated risk of depression.12 In Minnesota Questionnaire, according to data from the Cardiovascular Health Study, low weekly caloric expenditure means 383 or less Kcals/week for men and 270 Kcals/week or less for women.13
The subject or informant (in cases of cognitive impairment) were asked about the subject's history of falls in the last year (e.g., number, local and consequences of the last fall), using the definition of Chiu, Au-Yeung and Lo, (i.e., “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level and other than as a consequence of the following: sustaining a violent blow; loss of consciousness; sudden onset of paralysis; or an epileptic seizure”).15
Gait assessmentGait was assessed by using the 10-meter walk test. The test was chosen because it is a simple and quick tool to apply in clinical practice. Furthermore, this test has been associated with general health status and functionality, and the test can be used as an indicator of physiological reserve and risk of falls.16 The subjects were instructed to begin walking 1.2m before the beginning of the walk test course and to finish 1.2m after the end of the course at their usual gait speed. The subjects received the same standardized instructions.16 The test was conducted once, and the variables time (recorded using a stopwatch), number of steps, stops, gait speed (distance per time ratio in meter/seconds) and cadence (number of steps per time ratio in steps/minute) were measured. One assessor counted the number of steps and stops during the test. The test was standardized and all volunteers performed the test without any type of walking aid.
Dual task assessmentThe dual task was assessed using the Timed Up and Go Test (TUGT)17 associated with a motor-cognitive task (TUGT-DT).2 A single assessor conducted the test and gave the necessary commands.
Initially, the subjects performed the isolated cognitive-motor task. A raffled card (5×5cm) with eight numbers was fixed to a cordless phone (15.1-cm high×4.7-cm width×2.2-cm depth; Motorola FOX 1000 model) and placed on a table. The subjects received the following instructions while seated in front of the table: “Seated, pick up the phone, dial the numbers on the card and place the phone on the table. The starting command was: Ready, go”. “Pick up the phone”. “Dial”. After dialing or if the person did not dial, the command was: “Place the phone on the table” when the person finished the dialing or did not know the next task. The time was recorded after the command “go” and stopped when the elder placed the phone back on the table. Errors (i.e., incorrectly dialed number or an absence of any number being dialed) were marked.
The subjects performed TUGT after the isolated cognitive-motor task using a chair 45-cm high with trunk support and 68-cm-high armrests. The following instruction was given: “You will get up, walk the course, go back, and sit down. Ready, go”. “Get up”. “Walk”. “Go back”. “Sit down”. The time taken after the command “go” until the subject was seated against the trunk support again was recorded.
Subjects performed TUGT-DT using a newly drawn card (with eight numbers on it) fixed on the phone and the table positioned 50cm away from the chair. The subjects received the following instructions: “You will get up, pick up the phone, dial the numbers of the card while walking the course, place the phone on the table and sit down. Ready, go”. “Get up”. “Pick up the phone”. “Go on dialing while walking”. When the subjects reached the cone, they were told to: “Go back”. When the subjects reached the table, they were told to: “Place the phone on the table“. “Sit down”. The total time, number of steps, stops, cadence (steps/min), number of errors (i.e., incorrect dialed number or absence of any number), hits (i.e., correct dialed number)/time relation, motor task cost (%) and cognitive task cost (%) were analyzed. The last two variables were calculated according to Hall et al.18 and a positive value indicates percentage of decrement in performance under a dual task condition, whereas a negative value means percentage of improvement under a dual task condition.18 A single assessor counted number of steps and stops.
A pre-test was conducted by the assessor to allow the subjects to familiarize themselves with each of the tests and then each test was performed once on each subject. The assessor stayed behind the subjects during the test to prevent falls or injuries during the assessments. All subjects had satisfactory hand mobility, knew how to operate a telephone and recognized it as a phone19 to perform the isolated cognitive-motor task and the TUGT-DT Test. TUGT and TUGT-DT Tests were standardized and all subjects performed them without any type of walking aid.
Statistical analysisThe sample size was calculated using the G*Power 3.1 software (Universität Düsseldorf). A minimum of 108 subjects were necessary to constitute the total sample, assuming the type of study design, a type I error at 5%, statistical power at 80%, an effect size of 0.3 and a number of groups and response variables. Groups were paired using the Minnesota and GDS scores as these factors could influence the main variables studied.
A significance level of α=0.05 was adopted, and SPSS software was used (20.0). Data normality was tested using the Kolmogorov–Smirnov test. The ANOVA test (post hoc: Tukey test) and the Chi square test were used to analyze differences between groups for categorical data.
Significant between-group differences in age and gender were observed. The MANCOVA test (with age and gender as the confounding variables and Sidak as the correction adjustment for multiple comparisons) was used to compare gait and dual task performances between groups. A Chi-square test was used to compare history of falls and stops in TUGT-DT between groups.
ResultsThe sample consisted of 40 PC, 40 MCI and 38 AD elderly subjects (average time since diagnosis: 15 months). Table 1 presents the characteristics of the sample. There were differences between groups for age and gender. The AD Group presented a mean age up to four years older than the PC Group. There were more women (n=34) in the MCI Group compared to other groups. Other characteristics showed no difference between groups.
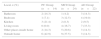
Sample characteristics for the sample of 3 test groups.
| Variable | PC Group (n=40) | MCI Group (n=40) | AD Group (n=38) | p value |
|---|---|---|---|---|
| Age (years), M±SD | 73.5±6.2+ | 75.8±6.3 | 77.7±6.2+ | 0.01 |
| Female gender, n (%) | 24 (60.0)+ | 34 (85.0)#,+ | 22 (57.9)# | 0.02 |
| Body mass index (kg/m2), M±SD | 29.3±5.7 | 29.4±4.2 | 27.3±5.3 | 0.14 |
| Abdominal Circumference (cm), M±SD | 100.4±13.1 | 101.4±11.5 | 98.9±13.4 | 0.70 |
| Education level (years), M±SD | 6.3±4.3 | 4.9±4.0 | 5.5±4.5 | 0.32 |
| Use of multi/bifocal glasses, n (%) | 25 (62.5) | 21 (52.5) | 14 (36.8) | 0.07 |
| Use of walking aids, n (%) | 4 (10) | 6 (15) | 4 (10.5) | 0.75 |
| GDS (0–15), M±SD | 2.7±2.7 | 4.0±2.7 | 3.8±2.6 | 0.07 |
| Minnesota, M±SD | 1389.4±1123.1 | 1458.2±2029.2 | 718.2±924.7 | 0.05 |
M±SD, mean±standard deviation; n (%), number of individuals (percentage of that group of subjects); PC, preserved cognition; MCI, mild cognitive impairment; AD, Alzheimer disease; kg/m2, kilograms per meter squared; cm, centimeters; GDS, Geriatric Depression Scale.
#,+ Difference between groups.
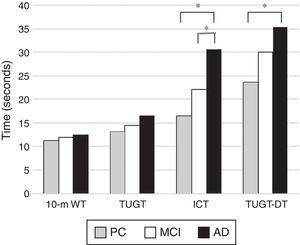
Table 2 and Fig. 1 present gait and dual task performances of the sample. There were no differences between groups for the 10-meter Walk Test for all variables investigated. All subjects performed the test in 11.9s and 19.8 steps on average, and all subjects completed the tests.
Gait and dual task performance scores for subjects with preserved cognition, mild cognition impairment & mild Alzheimer's disease.
| Variables (M±SD) | PC Group (n=40) | MCI Group (n=40) | AD Group (n=38) | F; p value |
|---|---|---|---|---|
| 10-m walk test | ||||
| Time (s) | 11.3±5.8 | 12.0±3.8 | 12.5±3.2 | 0.0; 0.934* |
| Steps | 18.7±6.3 | 20.4±5.6 | 20.5±4.3 | 0.2; 0.790* |
| Gait speed (m/s) | 0.9±0.2 | 0.8±0.2 | 0.8±0.2 | 1.5; 0.210* |
| Cadence (steps/min) | 103.2±13.5 | 103.5±14.4 | 100.0±11.0 | 0.3; 0.716 |
| Isolated cognitive task | ||||
| Time (s) | 16.5±4.6+ | 22.1±12.0# | 30.7±12.5#,+ | 15.1; 0.000 |
| Errors | 0.2±1.0+ | 0.3±1.0# | 2.7±5.9#,+ | 5.3; 0.006 |
| TUGT – time (s) | 13.1±6.0 | 14.4±4.5 | 16.6±5.0 | 2.4; 0.090* |
| TUGT-DT | ||||
| Time (s) | 23.6±9.8# | 30.0±14.6 | 35.4±13.7# | 5.4; 0.005* |
| Steps | 25.4±9.5 | 29.0±11.0 | 30.0±8.3 | 0.7; 0.455* |
| Stops, n (%) | ||||
| 0 | 4 (10.0) | 4 (10.0) | 0 (0) | 0.047a |
| 1–2 | 31 (77.5) | 28 (70.0) | 24 (63.2) | |
| >2 | 5 (12.5) | 8 (20.0) | 14 (36.8) | |
| Cadence (steps/min) | 65.8±11.3+ | 60.3±11.8# | 53.9±12.7#,+ | 10.7; 0.000 |
| Errors | 0.2±1.0+ | 0.8±1.7# | 2.8±4.0#,+ | 9.1; 0.000 |
| Hits/time | 0.3±0.1+ | 0.2±0.1# | 0.1±0.1#,+ | 15.1; 0.000* |
| Motor task cost (%)b | 87.0±60.7 | 103.1±44.5 | 112.7±57.3 | 1.9; 0.150 |
| Cognitive task cost (%)b | 23.6±34.5 | 33.4±19.9 | 30.2±32.7 | 0.3; 0.678 |
M±SD, mean±standard deviation; n (%), number of individuals (percentage of that group of subjects); PC, preserved cognition; MCI, mild cognitive impairment; AD, Alzheimer disease; m/s, meters/second; steps/min, steps/minute; TUGT, Timed Up and Go Test; TUGT-DT, TUGT dual task.
#,+,& Difference between groups.
Time spent on gait and dual task tests for subjects with preserved cognition, mild cognition impairment & mild Alzheimer's disease. PC, preserved cognition; MCI, mild cognitive impairment; AD, Alzheimer disease; 10-m WT, 10-meter walk test; TUGT, Timed Up and Go Test; ICT, isolated cognitive-motor task; TUGT-DT, TUGT dual task. *p<0.05.
In the Dual Task Test, the AD Group performed significantly worse in the isolated cognitive task both in time and number of errors than the other groups. The AD Group spent more time than the PC Group in TUGT-DT and had shorter cadence and more errors than the other groups. Most elderly subjects in the three groups had 1–2 stops in the TUGT-DT. However, more elderly subjects in the AD Group had more than 2 stops during the test compared to the other groups. No dual task variable measured could distinguish the PC from the MCI groups. There were no differences in time to do the TUGT and cognitive and motor task costs, which showed that the three groups had a decreased cognitive/motor performance under dual task conditions.
FallsAlthough there was a significantly higher percentage of fallers in the MCI and AD groups, there were no significant differences between groups in the number of falls (Table 3).
History of falls in the last year between groups for subjects with preserved cognition, mild cognition impairment & mild Alzheimer's disease.
| Variables, n (%) | PC Group (n=40) | MCI Group (n=40) | AD Group (n=38) | p value |
|---|---|---|---|---|
| Fallers | 14 (35.0)#,+ | 24 (60.0)# | 22 (57.9)+ | 0.04 |
| Number of falls, M±SD | 4.2±7.7 | 7.2±18.2 | 6.6±16.6 | 0.85 |
| Consequences presenteda | 9 (64.3) | 13 (54.2) | 6 (28.6) | 0.08 |
| Pain | 3 (21.4)# | 7 (29.2)+ | 0 (0)#,+ | 0.03 |
| Hematoma | 1 (7.1) | 7 (29.2) | 2 (9.5) | 0.12 |
| Hospitalization | 2 (14.3) | 1 (4.2) | 0 (0) | 0.16 |
| Knocked (hit) head | 1 (7.1) | 2 (8.3) | 2 (9.5) | 0.97 |
| Bleeding | 3 (20.0)#,+ | 0 (0)# | 1 (4.5)+ | 0.04 |
| Fracture | 2 (14.3) | 1 (4.2) | 0 (0) | 0.16 |
| Could not get up alone | 2 (14.3) | 5 (20.8) | 4 (19.0) | 0.88 |
n (%), number of individuals (percentage of that group); M±SD, mean±standard deviation; PC, preserved cognition; MCI, mild cognitive impairment; AD, Alzheimer disease.
#,+ Difference between groups.
All subjects reported that the latest fall was not accidental. Most elderly people with AD had no consequences. Verification of the consequences separately revealed that the MCI and PC groups were more likely to complain of more pain than the AD group (p=0.030). The PC Group also had more bleeding from the fall than the other groups (p=0.040) (Table 3).
There was no significant difference between groups in the location of the fall (i.e. inside or outside home). Specifically, 57.1% of PC, 62.5% of MCI and 85.7% of AD subjects fell in the home (Table 4).
Location of the latest fall among subjects who fell in the last year.
| Local, n (%) | PC Group (n=14) | MCI Group (n=24) | AD Group (n=22) |
|---|---|---|---|
| Bathroom | 2 (14.3) | 1 (4.2) | 3 (14.3) |
| Bedroom | 1 (7.1) | 3 (12.5) | 4 (19.0) |
| Kitchen | 3 (21.4) | 2 (8.3) | 2 (9.5) |
| Living room | 0 (0.0) | 4 (16.7) | 7 (33.3) |
| Other places inside home | 2 (14.3) | 5 (20.8) | 3 (14.3) |
| Outside home | 6 (42.9) | 9 (37.5) | 3 (14.3) |
n (%), number of individuals (percentage of subjects in that group); PC, preserved cognition; MCI, mild cognitive impairment; AD, Alzheimer disease; no difference between groups (p=0.24).
This study investigated differences in gait and dual task performances and history of falls between elderly volunteer subjects with PC, MCI and mild AD. The dual task, but not the simple gait test, differentiated the AD Group from the other groups, especially using the variables of the TUGT-DT. There was no difference between PC and MCI in any mobility performance. Elderly people with cognitive impairment had more falls than PC individuals. Specific characteristics in the history of falls between groups were identified.
The sample consisted of elderly volunteer subjects with low level of education, with no evidence of depression12 and no indication of low weekly caloric expenditure.13 No significant difference was found in abdominal circumference, use of bi/multifocal glasses, or walking aids between groups. Larger abdominal circumferences,20 related to a more central obesity and an unstable center of gravity, as well as poorer visual acuity,20 use of bi/multifocal glasses,21 use of walking aids indoors or outdoors,22 risk of depression22 and level of physical activity22 are associated with mobility impairment and falls in older people. Therefore, it was important to take into account these variables when analyzing our sample. Differences in age between groups was expected.1 In contrast to our findings, some authors have reported that the prevalence of MCI was higher in men.23,24 However, Lin et al.25 found that elderly women with MCI exhibited a faster progression of cognitive decline. The high prevalence of women with MCI in this study may be explained because Brazilian women look for more services involving routine examinations and prevention26 and have more memory complaints than men.27
There were no differences between groups in the 10-meter Walk Test or time spent on the TUGT. These tests are reliable outcome measures for people with AD.17 The three groups demonstrated better performance compared to a sample of older adults with mild to moderate AD, who performed the TUGT in 19.95s with a gait speed of 0.66m/s.17 When compared to healthy elderly people, our sample, mainly MCI and AD groups, showed impaired mobility, using a cut-off score of 1.0m/s16 for the 10-meter walk test and 10.2s28 for TUGT. However, there was a need for specific cut off scores to establish impaired mobility performances in older adults with MCI and mild AD.
In contrast to our findings, Eggermont et al.29 reported a decrease in performance on the Walk Test of elderly subjects with AD and MCI compared to PC, and the TUGT of elderly subjects with AD compared to PC. However, they used a 4-meter Walk Test without removing the acceleration and deceleration phases, had no familiarization, and the elderly with MCI and AD had more depressive symptoms. They also assessed elderly subjects with different phases of AD, and the sample had a higher education level compared to the present study. Studies with similar samples to the present study, using triaxial accelerometers, found differences in simple gait between AD and PC groups30,31 and AD and other groups,30 without any instruction during the mobility tests.
The three groups exhibited a decreased cognitive/motor performance under dual-task conditions, as seen by the values of cognitive and motor task costs far above zero.18 Gillain et al.30 also found no differences between groups in variations of dual task with single task performance, which could be interpreted similarly to task cost data. The dual task in the present study differentiated AD from the other groups, unlike simple mobility tests. The theory of shared resources of motor and cognitive control32 states that the motor alterations during walking are unmasked when the cognitive supply cannot meet the demand for performing physical function and the available cognitive resources are reduced in people with cognitive impairment.
The type of secondary cognitive task chosen seems to influence the identification of cognitive profiles in the elderly. Beauchet et al.33 reported that the countdown was the secondary cognitive task that most changed the kinematic parameters of gait. However, this finding is not clear in other studies, and the choice of secondary cognitive task seems to depend on which groups are differentiated in clinical practice, such as AD versus other groups or types of MCI versus other groups. Sheridan et al.5 demonstrated that tests involving frontal lobe functions were more compromised in elderly people with AD and were highly related to gait. Malouin et al.34 revealed an association between higher activity in some brain regions, including the prefrontal cortex and the hippocampus, with increasing complexity of gait. Our findings showed that this dual task with a functional secondary task involving executive function was efficient in differentiating AD from the other groups. Furthermore, the TUG-DT Test was easy and quick to use in clinical practice, even when applied to people with comprehension difficulties.
Other studies using dual task only considered the primary task (gait) and did not assess the secondary task.3,6 It is not known whether AD and MCI subjects prioritized the verbal task over the walking test without information about the separate task performance. In the present study, the AD Group performed the isolated cognitive task with significantly greater time and more errors than the other groups.
The high prevalence of falls in elderly people with MCI and AD compared to PC subjects was also seen in other studies.35,36 Borges et al.36 found that 57% of Brazilian elderly people with MCI and 65% of elderly people with mild AD reported falls in the last 12 months (retrospective data). The prevalence of falls in our sample could partially be related to the level of physical activity. In fact, there was an increase in the ratio of fallers (%) per physical activity based on the Minnesota Questionnaire (PC: 0.025; MCI: 0.0411; AD: 0.086) and the number of falls per physical activity (PC: 0.003; MCI: 0.004; AD: 0.009) according to cognitive profiles. Several other studies investigated risk factors for falls and their long-term consequences in elderly people with cognitive impairment,35,37 but there was a lack of studies that investigated the most common circumstances of falls in elderly people with MCI and mild AD and their immediate consequences. According to our findings, interventions to prevent falls should emphasize specific locations, such as adaptations in the living room, and in common functional activities performed in these locations for people with mild AD.
Guidelines for prevention of falls recommend that people with MCI undergo assessments and interventions based on evidence for elderly people without cognitive impairment.38 However, specific strategies for the screening and prevention of falls for each cognitive profile should lead to better positive effects.
This study has some limitations, such as the lack of restriction of an MCI type and the retrospective analysis of falls. Furthermore, although the assessor only performed each test once and a familiarization session was conducted for the isolated cognitive-motor task and the TUGT-DT Test, the familiarity with the phone model was not controlled. On the other hand, simple tools were easily used by the elderly subjects with cognitive impairment and were able to differentiate the groups. The authors adjusted the analysis for age and gender, which might have influenced mobility performance. The authors worried about the description of the test procedures and the use of standardized instructions, which could facilitate or reduce bias in mobility assessment of this population. Future research involving cutoff scores for each cognitive profile, different MCI types, validation of motor tests in cognitive impairment populations and prospective analyses of falls are necessary.
In conclusion, only the dual task test (TUG-DT) distinguished elderly people with mild AD from those with PC and MCI. None of the mobility tests performed could differentiate MCI from PC. Elderly subjects with cognitive impairment had more falls than PC individuals. Specific characteristics, including local and immediate consequences of falls, in each group were identified.
Conflicts of interestThe authors declare no conflicts of interest.
This study was supported by the Coordination for the Improvement of Higher Education Personnel (CAPES). The sponsor had no involvement in the study design, in the collection, analysis and interpretation of data.