A better understanding of performance in functional mobility tasks related to the mortality patterns for the different causes of death for the Brazilian older population is still a challenge.
ObjectiveTo analyze if gait speed and chair stand test performance are associated with mortality in older adults, and if the overall mobility status changes the effect of other mortality risk factors.
MethodsThe data were from SABE (Health, Well-being and Aging Study), a multiple-cohort study conducted in São Paulo, Brazil, with a representative sample of people aged 60 and more. Cox regression models were used to analyze 10-year all-cause and cause-specific mortality with consideration for gait speed and the chair stand test.
ResultsOf the 1411 participants, 26% died during the follow-up. The performance in the chair stand test had a more consistent association with mortality (hazard ratio (HR)=1.03, 95%CI: 1.00, 1.05) than gait speed. Being unable to perform the test also increased the risk to die by all-cause (HR=1.71, 95%CI: 1.21, 2.42) and by diseases of the circulatory system (HR=2.14, 95%CI: 1.25, 3.65). The stratified analysis of mobility performance changed the effects of some of the mortality risk factors, such as cognitive impairment and multimorbidity.
ConclusionsThe chair stand test could be a better choice than 3-meters walking test as a mortality predictor. In addition, the impact of cognitive decline and multimorbidity were greater among those with reduced mobility, supporting the development of preventive interventions and public policies targeted at more vulnerable groups of older adults.
In recent years, Brazil has experienced a significant rise in its older population.1 As the people age, the prevalence of mobility decline increases.2 Functional mobility comprises several functions necessary for the performance of activities of daily living and social participation. It can be defined as the ability to move independently from a place to another,3 and comprises functions that involve changing body position, carrying, moving or manipulating objects, walking, running, climbing, and even using transportation.4
There are many options to evaluate functional mobility. Simple physical performance tests, such as gait speed and the chair stand test, have been used as screening tool to identify older adults at risk for adverse health outcomes.5–8 The speed that an older person walks is sometimes considered the “sixth vital sign", an important marker of individual overall health status,7,9 and a relevant mortality risk factor.10 The ability to rise from a sitting position is also essential to functional independence, and to maintain a physically active life.11 The performance in this task is frequently used to assess lower limb function and to predict future health conditions such as falls and disabilities in older adults.6
The relationship of mobility disability with mortality is well established. However, there are still gaps in the literature regarding the effect of interactions between mobility decline and other risk factors. Some studies have indicated the negative impact of overlapped chronic conditions, such as frailty and other non-communicable diseases (NCD).12 Others have explored the consequences of the combination of mobility disability and cognitive decline.13,14 Nevertheless, a better understanding of the mortality patterns for the different causes of death, especially in terms of performance in functional mobility tasks, is still a challenge for the Brazilian older population.
The aim of this study was to analyze if gait speed and chair stand test performance are associated with all-cause and cause-specific mortality and if the overall mobility condition changes the effect of other mortality risk factors in older adults from São Paulo, Brazil.
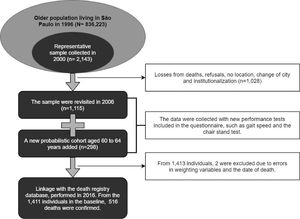
MethodsSample and data collectionThe data analyzed were from SABE (Health, Well-being and Aging Study), a multiple cohort study that is representative of older community-dwelling individuals living in São Paulo, Brazil. The first wave of SABE was conducted in 2000 as a multicenter study from 7 urban areas of Latin-America and Caribe and was coordinated by the Pan-American Health Organization (PAHO) and the Department of Epidemiology of School of Public Health of the University of São Paulo. The SABE study of the municipality of São Paulo, Brazil, is composed of a representative sample of people aged 60 years and more. In brief, individuals were selected by clusters from an initial sample of 72 census tracts, selected by a probability proportional to size approach. More details about the sampling strategy have been previously described.15 In São Paulo, a total of three other waves were collected in 2006, 2010, and 2015. In 2006, physical assessments such as gait speed were first added to the questionnaire, so this cohort was used as the baseline data for our analysis (n=1413). From this original sample, two individuals were excluded, one due to missing data related to the census tracts and the other due to incompatibility between the date of the interview and the date of death, resulting in 1411 individuals. The SABE Study received approval from the Human Research Ethics Committee of the School of Public Health/ Universidade de São Paulo, São Paulo, Brazil (protocol number 315/99, 83/06, and 2044) and all participants gave written informed consent.
OutcomesThe outcomes of interest were the death for all causes, and separately for the three most frequent causes of death, according to the 10th revision of the International Classification of Diseases (ICD-10): diseases of the circulatory system (I00-I99), diseases of the respiratory system (J00-J99), and neoplasms (C00-D48). The distribution of the mortality sample according to ICD-10 codes is presented in Supplementary material. Mortality data were obtained by a linkage between the SABE records and the death registry database from the Program for Improvement of Mortality Information in the Municipality of São Paulo (PRO-AIM), up to September 13th, 2016, totaling 10 years, with a maximum time of follow-up of 10.4 years. Individuals without mortality information were considered censored for the survival analysis. Fig. 1 shows the flow diagram of the study.
Variables of interestGait speed was evaluated by the time needed to walk a distance of 3 meters, with longer times reflecting worse performance. The 3-meter walk test is part of the Short Physical Performance Battery (SPPB),16 that evaluates lower body function. Gait speed was measured twice, and the shortest time was recorded. The following instruction was given to the participants: “This is our walking course. I want you to walk to the other end of the course at your usual speed, just as if you were walking down the street to go to the store.” The timer was started when the participant began to walk and stopped as soon as the participant completed the distance. The gait speed was calculated from the distance in meters divided by time in seconds and classified according to three categories: speed greater than 0.8 m/s, speed ≤0.8 m/s as having reduced gait speed,17 and being unable to perform the test (group composed mostly of bedridden or wheelchair-bound individuals, those who were physically unable to perform physical tests while standing or walking, and those who refused to perform the walk test because they felt unsafe).
The chair stand test is also part of the SPPB but widely used as a single test for measuring mobility disability and lower extremity function.5,16 Participants were asked to stand up from a chair 5 times consecutively as quickly as possible without hand support, and the time to complete the task was recorded (in seconds). The analysis with this variable was performed according to three categories (unable, time higher than 14 seconds, time equal or less than 14s). The cut-off point was proposed by Santos et al, 2016, based on a sample composed of Brazilian older adults.18
CovariatesOther independent variables included in models were age, sex, socioeconomic features (years of education [none, 1–3, 4–7, 8 or more years], race/skin color [white, black or mixed, others], and living alone [yes/no]), and the block of health variables (cognitive impairment [measured by the modified version of Mini-Mental State Examination, validated in a study conducted by Icaza and Albala,19 to minimize possible effects of low education on the test result], multimorbidity [the self-reported presence of two or more of the following diseases: hypertension, diabetes mellitus, musculoskeletal disorders (osteoarthritis, rheumatoid arthritis), cerebrovascular, pulmonary or cardiovascular diseases], alcohol intake [never, up to 1 day/week, 2 days/week or more], smoking status [never, currently, or have smoked before], and body mass index (BMI) [underweight, normal weight, overweight, or obesity] according to the PAHO, 200320).
Statistical analysisBaseline description of variables is presented in percentages for the whole sample and for the categories of the two mobility measures. The log-rank test to equality of survival curves was performed according to these factors. Continuous variables were described using means and standard deviations.
Cox regression models were performed to analyze the association between the independent variables and all-cause and specific mortality. Models adjusted by the block of socioeconomic variables, by the health variables, and by both were also performed. All models were adjusted by age and sex. Additionally, adjusted stratified models for the three different levels of functional mobility were fitted. The chair stand test was chosen for this analysis because it had a stronger association with mortality according to our results. The proportional hazard assumption of the models was tested by the Schoenfeld test. All analyses were performed considering sample weights with the survey package of R software (available in [https://cran.r-project.org/]).
ResultsA total of 1411 individuals were included in this study. Considering the complex sample design, 26% of the study population died during the 10-year follow-up: 39.3% by diseases of the circulatory system, 20.9% by neoplasms, and 17.0% by diseases of the respiratory system. Supplementary material shows the distribution of the sample according to the 3 most frequent ICD-10′s chapters. Mean age at baseline was 68 years, 59% were female, 58% had gait speed less than 0.8m/s, and 14% performed the chair stand test in more than 14 seconds (Table 1). Baseline characteristics of the sample according to socioeconomic, demographic and health variables, and the distribution of the sample according to gait speed and the chair stand test are provided in Table 1. From all individuals, 2.4% were excluded from the multiple analysis due to missing values (25 for BMI, 4 for education, 4 for alcohol intake, and 3 for ‘living alone’).
Sample distribution according to gait speed and chair stand test, n=1411.
| Variables | Total sample | Gait speed | Chair stand test | ||||
|---|---|---|---|---|---|---|---|
| Faster | Slower | Unable to perform | Faster | Slower | Unable to perform | ||
| Age (mean ±SD) | 69.6±7.5 | 67.8±5.5 | 69.9±7.6 | 73.2±10.3 | 68.2±5.5 | 69.1±7.4 | 75.1±9.4 |
| Sex | |||||||
| Female | 59.4 | 25.9 | 63.8 | 10.3 | 31.2 | 52.8 | 16.0 |
| Male | 40.6 | 39.9 | 50.0 | 10.1 | 42.5 | 46.0 | 11.5 |
| Living alonea | |||||||
| Yes | 13.2 | 18.7 | 72.6 | 8.7 | 36.7 | 49.9 | 13.4 |
| No | 86.8 | 33.6 | 55.9 | 10.5 | 30.1 | 50.6 | 19.3 |
| Education (years)a | |||||||
| None | 15.7 | 18.4 | 65.6 | 16.0 | 21.2 | 56.9 | 21.9 |
| 1 – 3 | 26.5 | 23.7 | 65.8 | 10.6 | 33.9 | 52.0 | 14.1 |
| 4 – 7 | 38.6 | 34.5 | 57.1 | 8.3 | 38.0 | 49.7 | 12.3 |
| >8 | 19.2 | 47.5 | 43.2 | 9.3 | 46.2 | 41.9 | 12.0 |
| Race/skin color | |||||||
| White | 63.4 | 33.5 | 56.0 | 10.5 | 35.6 | 49.2 | 15.2 |
| Black or mixed | 27.5 | 24.6 | 65.1 | 10.3 | 34.4 | 52.5 | 13.0 |
| Other | 9.1 | 39.4 | 52.5 | 8.1 | 41.2 | 48.8 | 10.1 |
| Multimorbidity | |||||||
| Yes | 55.6 | 26.1 | 61.8 | 12.2 | 29.8 | 51.7 | 18.5 |
| No | 44.4 | 38.5 | 53.6 | 7.8 | 43.2 | 48.0 | 8.7 |
| Alcohol intakea | |||||||
| Never | 69.2 | 25.3 | 63.0 | 11.8 | 31.5 | 51.2 | 17.3 |
| up to 1 day/week | 16.9 | 46.8 | 48.9 | 4.3 | 45.5 | 48.6 | 5.9 |
| 2 days/week or more | 13.9 | 44.3 | 45.9 | 9.8 | 45.3 | 46.3 | 8.5 |
| Smoking status | |||||||
| Current smoker | 14.0 | 30.4 | 58.3 | 11.3 | 38.9 | 48.1 | 13.0 |
| Former smoker | 34.0 | 29.1 | 60.7 | 10.2 | 37.6 | 46.7 | 15.6 |
| Never | 52.0 | 33.5 | 56.4 | 10.0 | 33.7 | 52.8 | 13.5 |
| Cognitive status | |||||||
| Impaired | 12.2 | 11.3 | 59.4 | 29.2 | 16.2 | 47.0 | 36.8 |
| Preserved | 87.8 | 34.4 | 58.0 | 7.6 | 38.5 | 50.5 | 11.0 |
| Body Mass Indexa | |||||||
| Low | 23.0 | 28.9 | 56.5 | 14.6 | 31.5 | 49.0 | 19.5 |
| Normal | 42.0 | 36.7 | 56.6 | 6.7 | 42.5 | 47.9 | 9.6 |
| High | 11.3 | 30.2 | 60.0 | 9.8 | 35.4 | 53.5 | 11.0 |
| Obesity | 22.1 | 27.5 | 66.2 | 6.3 | 30.0 | 57.0 | 12.9 |
| 10-year mortality | |||||||
| Yes | 25.9 | 21.0 | 60.9 | 18.1 | 25.1 | 48.9 | 26.1 |
| No | 74.1 | 35.3 | 57.2 | 7.5 | 39.5 | 50.5 | 10.0 |
| Gait speed | 0.79 ±0.26 | 31.6 | 58.2 | 10.2 | - | - | - |
| Chair stand test | 16.06±5.33 | - | - | - | 35.8 | 14.2 | 50.1 |
Data are percentages unless otherwise indicated
Table 2 presents the hazard ratios (HR) and 95% confidence interval (CI) according to baseline gait speed and chair stand test for all-cause and cause-specific mortality. It shows that gait speed had a negative association with all-cause mortality (HR=0.52, 95%CI: 0.30, 0.88) in the model adjusted by age and sex, but the association lost significance when adjusted by social and health variables. When analyzed as a categorical variable, slow gait speed was positively associated with all-cause mortality when adjusted by sex, age, and socioeconomic variables (HR=1.47, 95%CI: 1.09, 1.99 in Model 1, and HR=1.44, 95%CI: 1.06, 1.94, in Model 2), but not when adjusted by health features (Table 2).
Hazard ratios (HR) and 95% confidence intervals (CI) for 10-year mortality according to baseline gait speed and time to complete the chair stand test, n=1375a.
| Variables | Model 1b | Model 2c | Model 3d | Model 4e | |
|---|---|---|---|---|---|
| HR (95%CI) | HR (95%CI) | HR (95%CI) | HR (95%CI) | ||
| All-cause mortality | Gait speed (m/s) | 0.52 (0.30, 0.88)* | 0.59 (0.35, 1.00) | 0.67 (0.40, 1.13) | 0.68 (0.40, 1.15) |
| Chair stand test (s) | 1.03 (1.01, 1.05)⁎⁎ | 1.03 (1.01, 1.05)⁎⁎ | 1.03 (1.00, 1.05)* | 1.03 (1.00, 1.05)* | |
| Gait speed | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.47 (1.09, 1.99)* | 1.44 (1.06, 1.94)* | 1.19 (0.91, 1.56) | 1.33 (0.98, 1.82) | |
| Not able | 2.35 (1.64, 3.39)⁎⁎⁎ | 2.24 (1.54, 3.25)⁎⁎⁎ | 1.79 (1.20, 2.69)⁎⁎ | 1.80 (1.20, 2.70)⁎⁎ | |
| Chair stand test | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.42 (1.07, 1.88)* | 1.38 (1.04, 1.82)* | 1.39 (1.05, 1.85)* | 1.39 (1.05, 1.85)* | |
| Not able | 2.09 (1.52, 2.88)⁎⁎⁎ | 2.01 (1.46, 2.78)⁎⁎⁎ | 1.69 (1.19, 2.40)⁎⁎ | 1.71 (1.21, 2.42)⁎⁎ | |
| Mortality by diseases of the circulatory system | Gait speed (m/s) | 0.33 (0.12, 0.87)* | 0.40 (0.16, 0.99)* | 0.40 (0.16, 1.02) | 0.42 (0.16, 1.06) |
| Chair stand test (s) | 1.03 (0.99, 1.06) | 1.02 (0.99, 1.05) | 1.02 (0.99, 1.05) | 1.02 (0.99, 1.06) | |
| Gait speed | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.83 (1.10, 3.05)* | 1.74 (1.04, 2.90)* | 1.70 (1.01, 2.84)* | 1.64 (0.97, 2.77) | |
| Not able | 3.29 (1.81, 5.98)⁎⁎⁎ | 3.09 (1.69, 5.64)⁎⁎⁎ | 1.67 (1.02, 2.71)⁎⁎ | 2.44 (1.30, 4.56)⁎⁎⁎ | |
| Chair stand test | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.34 (0.86, 2.09) | 1.26 (0.81, 1.97) | 1.30 (0.83, 2.03) | 1.28 (0.82, 2.00) | |
| Not able | 2.75 (1.64, 4.61)⁎⁎⁎ | 2.52 (1.52, 4.18)⁎⁎⁎ | 2.14 (1.23, 3.70)⁎⁎ | 2.14 (1.25, 3.65)⁎⁎ | |
| Mortality by diseases of the respiratory system | Gait speed (m/s) | 0.64 (0.23, 1.77) | 0.82 (0.27, 2.44) | 1.22 (0.47, 3.16) | 1.24 (0.43, 3.56) |
| Chair stand test (s) | 1.03 (0.98, 1.08) | 1.02 (0.97, 1.07) | 1.02 (0.96, 1.08) | 1.02 (0.95, 1.08) | |
| Gait speed | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 0.86 (0.46, 1.59) | 0.81 (0.42, 1.57) | 0.65 (0.34, 1.23) | 0.66 (0.33, 1.30) | |
| Not able | 1.18 (0.61, 2.29) | 1.01 (0.48, 2.11) | 0.75 (0.37, 1.53) | 0.72 (0.35, 1.51) | |
| Chair stand test | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.28 (0.64, 2.54) | 1.23 (0.62, 2.46) | 1.21 (0.57, 2.53) | 1.23 (0.58, 2.60) | |
| Not able | 2.56 (1.25, 5.24)* | 2.45 (1.15, 5.23)* | 1.96 (0.92, 4.17) | 2.04 (0.94, 4.44) | |
| Mortality by neoplasms | Gait speed (m/s) | 0.42 (0.15, 1.20) | 0.46 (0.16, 1.26) | 0.40 (0.13, 1.20) | 0.39 (0.13, 1.18) |
| Chair stand test (s) | 1.04 (1.00, 1.08)* | 1.03 (0.99, 1.08) | 1.04 (1.00, 1.08)* | 1.04 (0.99, 1.08) | |
| Gait speed | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.92 (1.00, 3.65)* | 1.97 (1.05, 3.71)* | 1.84 (0.96, 3.54) | 1.98 (1.02, 3.86)* | |
| Not able | 1.19 (0.43, 3.30) | 1.14 (0.41, 3.15) | 1.09 (0.39, 3.06) | 1.10 (0.39, 3.10) | |
| Chair stand test | |||||
| Faster | 1.00 | 1.00 | 1.00 | 1.00 | |
| Slower | 1.61 (0.88, 2.95) | 1.57 (0.86, 2.84) | 1.65 (0.90, 3.03) | 1.61 (0.88, 2.93) | |
| Not able | 0.71 (0.31, 1.59) | 0.69 (0.30, 1.58) | 0.64 (0.28, 1.48) | 0.64 (0.27, 1.50) |
Regarding the time to perform the chair stand test, both the continuous and categorized variables maintained a significant association with all-cause mortality, even when adjusted by all variables. In the first model, adjusted by age and sex, the HR was 1.03 (95%CI: 1.01, 1.05), and in the model adjusted by age, sex, and socioeconomic and health features, the HR was 1.03 (95%CI: 1.00, 1.05). These associations were also observed with the chair stand test categorized by the cut-off point of 14s. The group that performed the test in >14 seconds had, on average, 39% higher risk to die than those who performed in a shorter time, with a 95%CI: 1.05, 1.85, independently from the demographic, socioeconomic, and health features (Table 2).
Not having performed both tests presented a consistent risk effect on all-cause mortality, with HR=1.80 (95%CI: 1.20, 2.70) for inability to perform the walking test, and HR 1.71 (95%CI: 1.21, 2.42) for inability to perform the chair stand test, adjusted by all blocks of variables. Regarding the cause-specific mortality, these inabilities were also associated with the risk to die by diseases of the circulatory system, even when adjusted by the co-variables (HR=2.44, 95%CI: 1.30, 4.56, for inability to carry out the walking test, and HR=2.14, 95%CI: 1.25, 3.65, for inability to perform the chair stand test) (Table 2). Regarding the other specific-causes of death, the results were less consistent across the models. These results are presented in Table 2.
Table 3 shows the HR of demographic, health, and socioeconomic models, stratified by mobility performance according to the chair stand test. The first model, that included those who performed the test in 14 seconds or less, found a negative association of alcohol consumption up to 1 day a week with all-cause mortality (HR=0.35, 95%CI: 0.16, 0.77). Also in the first model, smoking was an important mortality risk factor (HR=2.29, 95%CI: 1.24, 4.22), as well as in the second model that included individuals who performed the test in more than 14 seconds. In this second model, a positive association of being black or mixed-race (HR=1.73, 95%CI: 1.20, 2.49), and of cognitive impairment (HR=1.89, 95%CI: 1.26, 2.83) with mortality were found. In the last model, which included individuals who were not able to perform the test, the positive association with cognitive impairment remained, and an association with the presence of 2 or more non-communicable diseases was also significant (HR=1.75, 95%CI: 1.15, 2.67). Interestingly, in the last model, an inversion of the effect of being black or mixed-race was observed (HR=0.62, 95%CI: 0.41, 0.95).
Hazard ratios (HR) and 95% confidence intervals (CI) for 10-year mortality according to baseline socioeconomic and health variables stratified by categories of chair stand test, n=1411.
| Variables | Best performance (n=411) | Worst performance (n=698) | Not able (n=302) |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Age | 1.11 (1.07, 1.14)⁎⁎⁎ | 1.09 (1.07, 1.11)⁎⁎⁎ | 1.04 (1.02, 1.07)⁎⁎ |
| Sex (female) | 0.41 (0.23, 0.73)⁎⁎ | 0.56 (0.39, 0.81)⁎⁎ | 0.52 (0.34, 0.79)⁎⁎ |
| Race/skin color (ref.: white) | |||
| Black or mixed | 0.76 (0.43, 1.36) | 1.73 (1.20, 2.49)⁎⁎ | 0.62 (0.41, 0.95)* |
| Other | 0.83 (0.39, 1.77) | 1.21 (0.67, 2.18) | 1.13 (0.62, 2.05) |
| Multimorbidity | 1.05 (0.67, 1.65) | 1.10 (0.78, 1.55) | 1.75 (1.15, 2.67)⁎⁎ |
| Cognitive impairment | 1.20 (0.53, 2.74) | 1.89 (1.26, 2.83)⁎⁎ | 2.23 (1.49, 3.33)⁎⁎⁎ |
| Body mass index (ref.: normal) | |||
| Low | 1.34 (0.77, 2.34) | 1.46 (0.99, 2.15) | 1.48 (0.99, 2.20) |
| High | 0.93 (0.40, 2.18) | 1.41 (0.83, 2.38) | 0.49 (0.19, 1.25) |
| Obesity | 1.20 (0.61, 2.36) | 1.22 (0.77, 1.93) | 0.85 (0.46, 1.56) |
| Alcohol intake (ref.: never) | |||
| 0 or 1 day/week | 0.35 (0.16, 0.77)⁎⁎ | 0.81 (0.51, 1.28) | 0.78 (0.31, 1.96) |
| 2 days/week or more | 0.62 (0.32, 1.20) | 1.16 (0.67, 2.02) | 0.58 (0.32, 1.04) |
| Smoking status (Ref.: never) | |||
| Current smoker | 2.29 (1.24, 4.22)⁎⁎ | 2.37 (1.39, 4.06)⁎⁎ | 0.65 (0.33, 1.32) |
| Former smoker | 1.20 (0.70, 2.06) | 1.33 (0.89, 1.97) | 0.74 (0.49, 1.12) |
| Living alone | 0.53 (0.25, 1.11) | 1.37 (0.91, 2.07) | 1.52 (0.97, 2.36) |
| Years of education (ref: none) | |||
| 1 – 3 | 0.58 (0.28, 1.21) | 0.77 (0.50, 1.19) | 0.77 (0.47, 1.28) |
| 4 – 7 | 0.91 (0.47, 1.73) | 1.19 (0.76, 1.85) | 0.95 (0.57, 1.58) |
| >8 | 0.71 (0.35, 1.43) | 0.77 (0.39, 1.49) | 0.62 (0.31, 1.23) |
The present study aimed to analyze the mortality of older individuals according to mobility status, assessed by gait speed and by the chair stand test. Despite the fact that the association between gait speed and mortality was not significant for most statistical models, the time necessary to complete the chair stand test was a consistent mortality risk factor. Moreover, our results highlight that individual mobility condition could modify the effects of other mortality risk factors. For example, the average risk effects of cognitive impairment and multimorbidity are stronger in individuals with more impaired mobility.
Previous studies have shown that usual walking speed is a predictor of all-cause mortality, and some authors have suggested the routine use of this measure in clinical practice.21 White et al. analyzed trajectories of gait speed in older adults and found that the group with the fastest decline had a higher overall risk of death,8 however, they did not analyze interactions with other risk factors. Furthermore, other authors have used longer than 3 meter distances to assess gait speed,7,21–23 making it difficult to compare the findings.
Considering that shorter walks are more influenced by the acceleration phase, previous studies have recommended performing the gait speed test over distances longer than 4 meters.9 It may be the case that measures with longer distances are more associated with mortality, which could explain the non-significant association between all-cause mortality and reduced gait speed in the adjusted models. Similar results were found by Yu et al.13 who measured gait speed for a distance of 2.4 meters, in older community-dwelling individuals without cognitive impairment.13 Previous studies have suggested that tests of 3 or 4 meters could be used in case of limited spaces.9,24
Although gait speed is more studied as a predictor of mortality in older adults, in the present analysis the time to perform the chair stand test had a more consistent association with all-cause mortality risk. Another study conducted on 622 Italian older individuals has also shown that the time to perform the chair stand test was a better predictor of mobility disability than gait speed, even when measured over a distance of 7-meters.6 In contrast to the present study, Rolland et al.,25 found that the time to complete the chair stand test was not associated with mortality after adjustment by confounders.25 The authors included as covariates the ability to walk outdoors and instrumental activities of daily living, which could dilute the effect of mobility in the risk of death. Similar results were observed in a more recent study, in which the time to perform the chair stand test was also not associated with mortality after adjustment by covariates.26 In both studies, the follow-up period was shorter than the present study.
Regarding cause-specific mortality, gait speed presented bordering associations with death due to diseases of the circulatory system. Nofuji et al.,22 found an association of walking speed with mortality from cardiovascular diseases, but not from cancer, in a sample composed of Japanese older adults.22 In the present results, there was an association of slow gait speed and mortality by neoplasm in the fully-adjusted model.
It is interesting to note that the groups unable to perform both tests had an increased risk of death from all-causes and from diseases of the circulatory system, supporting the idea that people in the worst mobility condition are more vulnerable to adverse outcomes.27 On the one hand, mobility limitation increases the risk of sedentary behavior,28,29 which is associated to fatigue30 and higher incidence of cardiovascular diseases and diabetes.31 On the other hand, cardiovascular risk can predict frailty and mobility limitation.32 This two-way relationship could partially help to explain the causal mechanism of the increased mortality risk in the more disabled groups. Recent publications have highlighted the importance of increasing physical activity and reducing daily sitting time in the overall population. However, achieving the recommended goals can be very difficult for people with limited mobility,31,33 being a major challenge to be addressed in rehabilitation programs.
Our stratified analysis revealed that the functional mobility performance can modify the effects of mortality risk factors, such as cognitive impairment. Studies support that age-related mobility decline and cognitive function are strongly correlated, and that mobility decline could predict impairment in cognition.14 Evidences also confirm that cognitive impairment increases the risk of death in older adults, and this association could be stronger when cognition and mobility interact with each other.13,34
The presence of two or more NCD was more important as a mortality risk in the group with the worst mobility condition than in the other groups. The literature highlights the role of chronic diseases in triggering disabilities.35 However, there are complex mechanisms involving physical frailty and chronic diseases, such as cardiovascular events and diabetes, that help to explain these findings.36,37 Previous analyses have shown that multimorbidity is a risk factor for higher mortality, but it is subject to the number and combination of coexisting chronic diseases.38 According to our results, the combination of multimorbidity and mobility limitation also increases mortality risk. The concomitant presence of mobility decline with multimorbidity or cognitive impairment should be considered a priority in the allocation of individuals to specific preventive strategies and rehabilitation programs.
Health behaviors, such as smoking and alcohol consumption, were associated with mortality risk in the best mobility groups. There is a lot of evidence that heavy drinkers have a higher risk of death, however, some studies have shown that moderate alcohol use is associated with overall better health,39 and therefore with a lower risk of death,40 as observed in our results. It is worth mentioning that measuring unit/day consumption, as performed by Ortolá et al.,41 was not possible in this present study which limits the interpretation of the results.
Having a current smoking habit presented a risk effect on all-cause mortality in the groups that performed the chair stand test. Smoking is an important and consistent mortality risk for the overall population and also for older adults.42 Both alcohol consumption and smoking were measured only at baseline, so the changes over time until the end of follow-up were not assessed. Considering the time-dependent characteristic of these variables could help explain our results, especially given the fact that there is no risk-free level of exposure to tobacco smoke.42
Some social aspects did not present significant associations in the stratified analysis; however, being black or of mixed racial background was positively associated with mortality in the slowest group, but negatively in the unable group. Historically, black and mixed racial background individuals have been at social disadvantage worldwide, and according to the literature, they have a higher risk of death and other adverse health outcomes.43,44 However, opposite to what was expected, being black and of mixed racial background had a protective effect against mortality among the group unable to perform the chair stand test. Latham et al.45, also observed that black individuals were more likely to recover their mobility than Whites.45 Nevertheless, some aspects should be considered before interpreting our result. First, a selection bias could have influenced the baseline characteristics of the sample, because the study was not designed to be representative of race/skin color.44 Second, the possibility of bias due to the presence of mortality before the baseline interview cannot be excluded, as life trajectories of disabled people according to race could explain this result. However, the importance of giving special attention to the health of black and mixed racial background individuals, especially if they are in the worst mobility condition should be highlighted.
This study has some limitations. First, mortality data were obtained by linkage, so the existence of a few missing individuals cannot be ruled out. To avoid this, we manually checked all detected pairs. Second, some variables such as the presence of NCD, were self-reported. To avoid memory bias, we questioned everyone from the sample if a health professional ever told them they had each specific disease (e.g. “Did a doctor or nurse ever tell you that you have Diabetes Mellitus?”). However, there is the issue of the presence of non-diagnosed diseases, so these results could be underestimated. Third, a dose-response relationship for some of the categorical variables was not found, and the possibility of unmeasured potential confounders cannot be excluded. Fourth, the distance measure for gait speed was shorter than for some published papers, being likely less sensitive to small changes in mobility status. Nevertheless, it allowed the assessment of walking time in a community-dwelling sample of a large and socially unequal city, where individuals do not always have enough space in their homes.
ConclusionThe present study brings new insights concerning mortality patterns from an ethnic and socioeconomic diverse population by all-cause and cause-specific mortality. More specifically, the chair stand test could be a better choice than 3-meters walking test as a mortality predictor. This finding is especially interesting when there is little space available, as observed in some homes and health units. The presented results support the development of rehabilitation programs, preventive interventions, and public policies targeted at more vulnerable groups of older adults, such as people with poorer mobility combined with cognitive decline or multimorbidity. The need for special attention to groups with poorer mobility should be highlighted because their difficulty in locomotion puts them at a disadvantage in accessing public health services. Lastly, these findings also contribute to organizing effective screening and allocation of individuals, especially in primary health care.
This work was supported by the Brazilian National Research Council (CNPq) [grant number 152494/2016-2].