Previous studies have shown positive results of phototherapy for improving performance and accelerating recovery; however, the effects of phototherapy during training and after a primary adaptation remain unclear. The aim of this randomized controlled trial is to analyze the effects of phototherapy and combined training on clinical, functional, and psychological outcomes and on vascular endothelial growth factor.
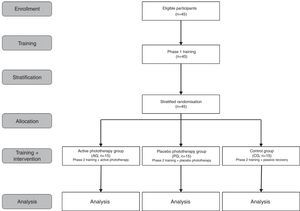
MethodsThis randomized placebo-controlled trial by stratified sample will involve 45 healthy male participants. In phase 1, the participants will undergo six weeks of combined training (sprints and squats). In phase 2, participants will be allocated through stratified randomization (based on adaptation capacity) into three groups: active phototherapy group (AG), placebo group (PG), and non-treatment control group (CG). A new six-week training program will then start and the participants will receive the recovery strategy between sprints and squats. The primary outcome will be maximal isometric contraction. The secondary outcomes include strength and power testing, maximal incremental test, squat jump, sprint test, muscle soreness, pain threshold, perceptions of exertion and recovery, psychological questionnaire, and vascular endothelial growth factor.
ConclusionsThis will be the first trial to include phototherapy during training. We believe that this strategy will combine the ergogenic and prophylactic effects in the same session. Furthermore, an application protocol performed after primary adaptation may reflect the real effect of the technique.
Phototherapy has been the focus of important research in sports science in recent years.1 Also known as the phenomenon of photobiomodulation or photobiostimulation,2 this technique is the application of monochromatic light that can influence cellular activity through inhibition or stimulation of chemical and biological functions.3 Phototherapy has two main light sources, i.e., laser and LED (light emitting diode), that are applied separately and, in recent years, in combination, and has demonstrated a significant therapeutic advance with subsequent clinical improvement.4
Experimental studies and clinical trials have identified the possible physiological effects of this technique on muscle tissue undergoing structural or metabolic stress.5 The main findings showed the formation of giant mitochondria able to provide high respiratory rates, a higher volume of energy, and greater mitochondrial density in the tissues6 with consequent synthesis of adenosine triphosphate (ATP),7 modulation of gene expression with regeneration of musculoskeletal tissue,5 increases in local microcirculation8 and modulation of endothelial function with angiogenesis upregulated by the technique with vascular endothelial growth factor (VEGF) as mediator.9,10 These interactions have repercussions in exercise and its mechanisms of action are related to two main effects, i.e., ergogenic and protective or prophylactic.11 Borsa et al.11 relate the ergogenic effects of changes in microcirculation, reduction in lactic acid production,12–14 improvement in mitochondrial function, and increase in antioxidant capacity.15–17 The protective effect is closely related to muscle cell protection against muscle damage,17 producing anti-inflammatory and antioxidant effects.11
From these mechanisms, positive results can be observed in a range of outcomes, as discussed in recent systematic reviews3,11 and clinical trials.4,12,14–23 The magnitude of the effects of phototherapy can be influenced by the different application techniques, such as wavelength, energy density, and power, as well as the type of damage and time of application.3,24 Recent studies3,4 have aimed to eliminate these potential biases by identifying the best management application. Regarding the time of application, Leal-Junior et al.3 emphasize that 92% of the studies included in a systematic review opted to apply the technique before exercise. However, studies have shown positive effects on different markers from application both before and after exercise, although no justification for such a choice is given other than author preference.
Thus, investigation into the management of phototherapy adjusted to a model of training (between structural and metabolic exercise), could combine the ergogenic and protective effects in the same session. In addition, phototherapy applied after control of the primary adaptation to exercise may reflect the real effect of the technique. Thus, the objective of the study is to analyze the effect of phototherapy with different light sources (low-level laser therapy and light-emitting diodes) and combined training on clinical, functional, and psychological outcomes and on vascular endothelial growth factor. Accordingly, the study hypothesis is that the use of a phototherapy protocol, adjusted to a specific time of physical stress, will lead to significant improvements in the recovery process and in damage prevention.
MethodsStudy design and settingsWe will conduct a randomized, placebo-controlled clinical trial with parallel groups at Universidade Estadual Paulista (UNESP), Presidente Prudente, SP, Brazil. The trial has been prospectively registered at ClinicalTrials.gov (NCT02918916) and approved by Human Research Ethics Committee of UNESP, Presidente Prudente, SP, Brazil (1.389.046/2016). The study follows the SPIRIT 2013 checklist (Standard Protocol Items: Recommendations for International Trials)25 and TIDieR (Template for Intervention Description and Replication)26 to improve the information and quality of intervention reporting.27 Prior to the procedures, the participants will receive oral and written instructions and sign a consent form agreeing to participate in the study. All personal data will be confidential.
Participants will undergo a 12-week training program divided into two phases. In phase 1 (six weeks), participants will undergo training consisting of sprints and squats in the same session. After this period, the participants will undergo new tests and be randomly allocated into the groups that comprise the study. In phase 2, a new six-week training period will begin. In this phase, the participants will train normally with the adjusted loads and between sprints and squats will receive the recovery strategy related to the group to which they belong.
A flowchart of the design, composition of the groups, and phases is presented in Fig. 1.
ParticipantsA total of 45 healthy male volunteers will be recruited from the local university (UNESP) via online media advertisement, personal invitation, telephone, and SMS and registered in the database of the Sports Physical Therapy Laboratory. These procedures are recommended by Treweek et al.28 as a strategy to improve participant recruitment.
Initial contact with all participants will be made by telephone to establish their willingness to participate and a meeting will be scheduled to evaluate the eligibility criteria.
The following inclusion criteria will be employed:
- •
Healthy patient (self-report);
- •
Male gender;
- •
Age between 18 and 30 years.
Participants with the following will be excluded from the study:
- •
History of cancer;
- •
Presence of anemia, inflammation, or diabetes;
- •
History of muscle injury in the lower limbs or spine in the previous six months.
- •
Occurrence of musculoskeletal injury during the study.
Participants will be instructed to maintain their daily diet routine and abstain from anti-inflammatory and analgesic drugs, as well as any exercise not presented during the study. This information will be reinforced during data collection and monitored by self-report to further analysis.29
Randomization proceduresParticipants will be randomly allocated to the groups after phase 1. The stratification process will be carried out based on the concept of responders and non-responders to adaptation capacity,30 defined in this study as functional and clinical responses. Each response will be recorded before and after phase 1.
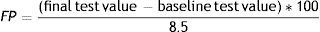
Adaptation capacity (AC) will be extracted using the following equation:
Functional parameter (FP)A priori knowledge will be used based on the study of Kotzamanidis et al.,31 who observed average gains of 8.5% after combined training. This value is set as the ceiling of strength gain capacity. Therefore, gains ≥8.5% in strength test will correspond to 100% of FP and gains <8.5% will be inserted into the following equation:
Clinical parameter (CP)The perception of recovery will be assessed using a 10-point Likert scale.32 Each point on the scale is considered as 10% of CP. Participants will be evaluated at the end of session 10.
Participants will be stratified into three strata based on their adaptation capacity:
- -
Participants with AC values below the median;
- -
Participants with AC values between the median and the 3rd quartile;
- -
Participants with AC values above the 3rd quartile.
A block randomization33 with blocks of three will be used to allocate participants of each stratum. Participants will be allocated to groups in a 1:1:1 ratio into the following groups: active phototherapy group (AG), placebo phototherapy group (PG), and control group (CG).
To ensure allocation concealment, randomization to groups will be undertaken by an independent researcher who will be instructed not to inform the participants or other researchers.34
Details of proceduresTraining programThe training program will be based on combined training described by Marques et al.35 The program is considered individualized and based on a load moved in 1ms−1 in a strength and power test.
The training consists of a combination of maximal sprints and explosive squats. Sessions will be held twice a week (48-hour interval) for six weeks, followed by a second six-week program. Phase 1 of the training program (six weeks) aims to induce adaptation and making the participants’ level of physical activity more uniform. Phase 2 corresponds to the experimental phase, in which the recovery strategies will be given following stratified randomization.
The reference study35 and a pilot study did not show any adverse effects from training. However, the adherence or adverse events will be recorded for further analysis. To improve adherence to the protocol, the participants will receive telephone reminders or SMS messages.28
A detailed description of the training program is presented in Table 1.
Training program.
| Phase | Week | Sessions | Sprint training | Squat training | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Warm up* | Intensity† | Sets×Repetitions | Rest between sets | Warm up* | Intensity† | Sets×Repetitions | Rest between sets | ||||
| Phase 1 | 1 | 1 | 3×20m | Maximum | 2×15m | 120s | 10min between training | 1×8+1×8 | 80% | 1×8 | 120s |
| 2 | 3×20m | 2×15m | 120s | 1×8+1×8 | 80% | 2×8 | 120s | ||||
| 2 | 3 | 3×25m | 2×20m | 120s | 1×8+1×8 | 85% | 1×8 | 120s | |||
| 4 | 3×25m | 2×20m | 120s | 1×8+1×8 | 85% | 2×6 | 120s | ||||
| 3 | 5 | 3×30m | 2×25m | 150s | 1×8+1×8 | 90% | 1×6 | 120s | |||
| 6 | 3×30m | 2×25m | 150s | 1×8+1×8 | 90% | 2×8 | 120s | ||||
| 4 | 7 | 3×35m | 2×30m | 180s | 1×8+1×6 | 95% | 1×6 | 180s | |||
| 8 | 3×35m | 2×30m | 180s | 1×8+1×6 | 95% | 2×5 | 180s | ||||
| 5 | 9 | 3×25m | 2×20m | 150s | 1×8+1×6 | 100% | 2×6 | 180s | |||
| 10 | 3×25m | 2×20m | 150s | 1×8+1×6 | 100% | 2×5 | 180s | ||||
| 6 | 11 | 3×30m | 1×25m | 180s | 1×8+1×6 | 90% | 2×6 | 120s | |||
| 12 | 3×30m | 1×25m | 180s | 1×8+1×6 | 80% | 1×8 | 120s | ||||
| 7 | Interval between phasesΔ | ||||||||||
| Phase 2 | 8 | 13 | 3×20m | Maximum | 2×15m | 120s | 10min between training | 1×8+1×8 | 80% | 1×8 | 120s |
| 14 | 3×20m | 2×15m | 120s | 1×8+1×8 | 80% | 2×8 | 120s | ||||
| 9 | 15 | 3×25m | 2×20m | 120s | 1×8+1×8 | 85% | 1×8 | 120s | |||
| 16 | 3×25m | 2×20m | 120s | 1×8+1×8 | 85% | 2×6 | 120s | ||||
| 10 | 17 | 3×30m | 2×25m | 150s | 1×8+1×8 | 90% | 1×6 | 120s | |||
| 18 | 3×30m | 2×25m | 150s | 1×8+1×8 | 90% | 2×8 | 120s | ||||
| 11 | 19 | 3×35m | 2×30m | 180s | 1×8+1×6 | 95% | 1×6 | 180s | |||
| 20 | 3×35m | 2×30m | 180s | 1×8+1×6 | 95% | 2×5 | 180s | ||||
| 12 | 21 | 3×25m | 2×20m | 150s | 1×8+1×6 | 100% | 2×6 | 180s | |||
| 22 | 3×25m | 2×20m | 150s | 1×8+1×6 | 100% | 2×5 | 180s | ||||
| 13 | 23 | 3×30m | 1×25m | 180s | 1×8+1×6 | 90% | 2×6 | 120s | |||
| 24 | 3×30m | 1×25m | 180s | 1×8+1×6 | 80% | 1×8 | 120s | ||||
Recovery strategies will be applied between sprint and squat training. We chose this moment of application because of the possibility of associating ergogenic and protective effects of phototherapy in the same session.
A trained therapist will apply active phototherapy bilaterally using the MR4 LaserShower 50 4D emitter (Multi Radiance Medical, USA) to six sites on the quadriceps (two centrally – rectus femoris and vastus intermedius; two laterally – vastus lateralis; two medially – vastus medialis) in direct contact with the skin. The option to apply phototherapy at these sites was chosen due to this muscle group being more directly involved in squats and the most worked during sprints. To receive intervention, the participant will be placed in the supine position. Phototherapy parameters are described in Table 2.
Phototherapy parameters.
| Number of lasers | 4 super-pulsed infrared |
| Wavelength (nm) | 905 |
| Frequency (Hz) | 250 |
| Peak power (W) – each | 12.5 |
| Average mean optical output (mW) – each | 0.03125 |
| Power density (mW/cm2) – each | 0.07 |
| Dose (J) – each | 0.07125 |
| Spot size (cm2) – each | 0.44 |
| Number of red LEDs | 4 red |
| Wavelength (nm) | 640 |
| Frequency (Hz) | 2 |
| Average mean optical output (mW) – each | 15 |
| Power density (mW/cm2) – each | 16.66 |
| Dose (J) – each | 3.42 |
| Spot size (cm2) – each | 0.9 |
| Number of infrared LEDs | 4 infrared |
| Wavelength (nm) | 875 |
| Frequency (Hz) | 16 |
| Average mean optical output (mW) – each | 17.5 |
| Power density (mW/cm2) – each | 19.44 |
| Dose (J) – each | 3.99 |
| Spot size (cm2) – each | 0.9 |
| Magnetic field (mT) | 35 |
| Irradiation time per site (s) | 228 |
| Total dose applied (J) | 180 |
| Aperture of device (cm2) | 20 |
The optical power will be calibrated before irradiation in each participant using a Thorlabs thermal power meter (Model S322C, Thorlabs, Newton, NJ, USA) and the dosage applied will be 30J per site (180J per muscle). This dosage is considered the optimal dose to improve performance, muscle soreness, and biochemical markers related to skeletal muscle damage.4
The same procedures as in the active phototherapy group will be applied to the placebo group; however, the emitter will be disabled. The device will emit the same sounds regardless of the programmed mode (active phototherapy).
The control group participants will remain seated for passive recovery supervised by an independent therapist36 during the period when the other groups are receiving recovery strategies.
Primary and secondary outcome measures and assessment pointsThe primary outcome will be the peak torque obtained in the maximal voluntary isometric contraction. Secondary outcomes are other functional, clinical, and psychological outcomes and VEGF, described below. Data will be collected in a specific time point (Table 3). Each assessor will be responsible for the same outcome throughout the study. Performance tests will be completed in two sessions separated by a day of rest and will be performed in the order described below.
Time point of outcomes.
| Outcomes | Time point | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SW* (phase 1) Stratification analysis Before adaptation | SW* (phase 2) Recovery effect After adaptation | ||||||||||||
| M1 | M2 | M3 | M4 | M5 | M6 | M7 | M8 | M9 | M10 | M11 | M12 | ||
| Performance tests | Strength and power tests | ✓ | ✓ | ✓ | |||||||||
| Maximal voluntary isometric contraction | ✓ | ✓ | ✓ | ||||||||||
| Maximal incremental test | ✓ | ✓ | ✓ | ||||||||||
| Squat jump | ✓ | ✓ | ✓ | ||||||||||
| Sprint test | ✓ | ✓ | ✓ | ||||||||||
| Muscle soreness | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Pain threshold | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Perception of exertion | ✓ | ✓ | ✓ | ✓ | |||||||||
| Perception of recovery | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Psychological questionnaire | ✓ | ✓ | ✓ | ||||||||||
| Belief questionnaire | ✓ | ✓ | |||||||||||
| Vascular endothelial growth factor | ✓ | ✓ | ✓ | ||||||||||
SW, specific week (phase 1: session 9 and 10; phase 2: session 21 and 22).
M1: baseline; SW (phase 1)=M2: before training; M3: after sprint training; M4: after complete training; M5: 60min after complete training; M6: after phase 1. SW (phase 2)=M7: before training; M8: after sprint training; M9: after recovery strategy; M10: after complete training; M11: 60min after complete training; M12: after phase 2.
In the first session, the sprint test, squat jump, and maximal incremental test will be completed. In the second session, the strength and power tests and maximal voluntary isometric contraction (MVIC) will be performed. Additionally, care will be taken to allow sufficient rest (15min) between all tests on the same day to limit the effects of fatigue on the following test. This rest is based on time to recovery of each test.37–41
Primary outcomeMaximal voluntary isometric contraction (MVIC)Participants will be positioned with the dominant leg on the isokinetic dynamometer (Biodex System 4 Pro, New York, USA). Prior to the MVIC, they will do a warm up consisting of 10 repetitions of knee flexion–extension at 180°s−1 throughout the range of motion. The MVIC will be determined by the highest maximal isometric torque over three contractions of five seconds at 60° of knee flexion. The repetitions will be separated by a 2-min rest interval.17
Secondary outcomesThere will be 12 secondary outcomes to understand the comprehensive process of post-exercise recovery and performance.
- •
Strength and power testing: these tests will be carried out with a bar.35 Participants starting in the upright position with the bar in contact with the shoulders and will be required to perform the squat with continuous movement until their thighs reach the horizontal plane, then immediately perform the reversed motion at maximum speed. Information about the eccentric distance reached and concentric speed of each repeat will be recorded by a linear velocity transducer (T-Force System Ergotech, Murcia, Spain), which will also provide visual and auditory feedback.
For the strength test, the warm up will consist of 10 repetitions at 40–60% of maximum perception. The last acceptable repetition with the highest possible load will be considered 1RM (repetition maximum). The rest period between sets is two minutes.
To determine the velocity of displacement during the concentric phase of full squat, the load will be adjusted until the highest velocity is obtained. The velocity index is calculated by the average value of peak velocity obtained with each load. The tests will be carried out gradually and with increments of 10kg for each set with two trials executed with each load.
For the power test, the warm up will consist of five repetitions with the bar. Bar displacement and peak and mean velocity will be recorded by an encoder. A computer program (Isocontrol Dinámico, 3.6, Spain) will be used to calculate the velocity of displacement for each repetition throughout the range of motion. An interval of 2–3min will be given between trials. The best trial with each load will be recorded.
- •
Maximal incremental test: the maximum oxygen consumption (VO2max) and maximum aerobic speed (MAS) will be determined on a treadmill (Inbramed, Inbrasport, Brazil) using an incremental protocol.42 Participants will do a five-minute warm up at 7kmh−1. After five minutes of rest, the participants will perform the incremental protocol consisting of running at a starting velocity of 10kmh−1, with increments of 1kmh−1 per minute until exhaustion and a fixed inclination of 1%. The test will finish through voluntary exhaustion or the presence of clinical alterations. Gas analysis will be measured continuously and the average value of every 30s will be recorded (VO2000, MedGraphics, Minnesota, USA). The MAS will be recorded as the speed corresponding to the final complete step in the incremental test.
- •
Squat jump: participants will remain with the sole of their feet in contact with the jump platform (Multisprint, Hidrofit, Brazil), legs at 90° of flexion, hands on hips, trunk upright, and without previous movements. The participant will perform a jump keeping their legs straight (180°) and touch the platform again. Each participant will perform three complete tests with a 30-second rest interval.43 The best measure of the tests will be adopted.
- •
Sprint test: participants will perform three maximum sprints exceeding 30m with 3-min rest intervals. Performance times at 10, 20, and 30m will be recorded (Multisprint, Hidrofit, Brazil).35 The average of the two best tests will be adopted.
- •
Muscle soreness: values of muscle soreness in lower limbs will be obtained through an 11-point visual analog scale (VAS),17 with ‘zero’ corresponding to absence of soreness and ‘10′ to the maximum level supported by the participant.44
- •
Pain threshold: pressure algometry will be applied at five specific sites of the quadriceps in the dominant leg.45 Participants will be instructed to signal when the pressure sensation becomes discomfort. The pressure will not exceed 2.55kgf.46
- •
Perception of exertion: the level of exertion reported by participants will be assessed using the Borg Scale (6–20 points), with ‘six’ corresponding to ‘very easy’ and ‘20′ to ‘exhaustive’.47
- •
Perception of recovery: the level of perception of recovery will be assessed by a 10-point Likert scale, with ‘one’ corresponding to ‘not recovered’ and ‘10′ to ‘fully recovery’.29,32
- •
Psychological questionnaire: participants will be instructed to mark an “X” on a 10-cm visual analog scale, with ‘zero’ corresponding to ‘least possible’ and ‘10′ ‘most possible’ for each rating (readiness for exercise, fatigue, vigor, sleepiness, and pain).48
- •
Belief questionnaire: after phase 1, participants will answer a belief questionnaire to measure their ‘belief’ in the effectiveness of the technique. Participants will be instructed to mark an “X” on a 5-point Likert scale, with ‘zero’ corresponding to ‘not effective’ and ‘10′ to ‘extremely effective’. After application of the recovery techniques, the participants will complete a similar questionnaire to measure their perceived effectiveness of the technique.48
- •
Vascular endothelial growth factor (VEGF): 10ml of blood will be collected and plasma from this sample will be stored at −80°C for later analysis. The plasma level of VEGF will be analyzed using the ELISA method (enzyme-linked immunosorbent assays) following the manufacturer's instructions (RayBio, Norcross, GA, USA).49
This study will ensure that assessors will be blinded. Although the therapist is not blinded, he will not have access to which recovery strategy is being applied (phototherapy or placebo). One participating researcher will be responsible for programming the phototherapy device based on random allocation. In this study design, it will not be possible to blind the participants and therapists due to the control condition.
Sample size calculationsBased on data from a previous study4 that used the same light source of phototherapy, for a three-arm parallel study (with SD=38.86Nm on MVIC with α=0.05 and β=0.8, to detect a difference of 10%) a total sample of 45 will be required, allowing for sample loss.
Statistical analysisThe statistical analysis will be conducted in SPSS (version 18; SPSS Inc., Chicago, IL, USA). After the adaptation process, the data will be analyzed as described below.
For outcomes with two time points: analysis of covariance (ANCOVA) with general linear models will be used to test between-group differences, with the difference/delta value as a dependent factor, group variable as fixed factor, and baseline values as covariate. (Outcomes: performance tests, VEGF, belief questionnaire, perception of exertion.)
For outcomes with three or more time points: initially, sphericity of the data will be tested by Mauchly's test. In case of violation of the sphericity assumption, the Greenhouse–Geisser corrections will be used. Analysis of variance (ANOVA) with repeated measurements will be used to test between-group differences followed by Bonferroni or Dunn post hoc test. (Outcomes: perception of recovery, psychological questionnaire, muscle soreness, and pain threshold.)
The data will be double entered. All participants will be included in the analyses following an intention-to-treat approach and the significance level will be set at p<0.05.
DiscussionPhototherapy is a strategy commonly used by physical therapists to minimize the changes caused by exercise, promote post-exercise recovery, and improve performance. However, different application times have been used. A recent review3 showed that 92% of included studies chose phototherapy before exercise, but it did not justify the choice. However, evidence has shown positive effects in the application before and after exercise in the ability to prevent injuries related to muscle fatigue and also in the improvement of the recovery process.3,4,50 Thus, the building of a rationale based on adjustment of phototherapy to training seems relevant. We believe that this strategy could combine the ergogenic and prophylactic effects of phototherapy in the same session. Furthermore, an application protocol performed after control of the primary adaptation process resulting from the exercise may be able to reflect the real effect of the technique.
This trial will contribute to evidence-based use of phototherapy in training programs, providing a better understanding of the technique and improved logistics for the recovery process. It contemplates the items of checklists for protocol studies to minimize bias, and it was prospectively registered. We chose to perform randomization with stratification by adaptation process to improve the methodological quality of the study. To achieve this, we will use measures of performance and perception of recovery. As this strategy has not yet been conducted, it is not possible to infer about its full efficiency, and such condition may represent a potential limitation. Data will be published after the study is completed.
Conflicts of interestProfessor Ernesto Cesar Pinto Leal-Junior receives research support from Multi Radiance Medical (Solon, OH, USA), a laser device manufacturer. The remaining authors declare that they have no conflict of interests.
The authors wish to thank the São Paulo Research Foundation (FAPESP process numbers 2015/25220-9 and 2015/25219-0) and the National Council of Technological and Scientific Development (CNPq) for their financial support.