To develop and analysis of measurement properties an instrument to assess maternal perception of fatigue during childbirth.
MethodsThe study was developed in three steps: elaboration of the initial version of the questionnaire from literature review and semi-structured interviews of the health professionals and the women during labor; consultation of Brazilian specialists through a Delphi Study, to define the items that should compose the final version of the document; validation and factor analysis.
ResultsA 51-item questionnaire, comprised of the perception of general health, physical, emotional and cognitive aspects of the parturient was composed through both literature search and the interview of health professionals and women during labor. The Delphi Study was composed of three rounds and the instrument was reduced to 12 questions by its end, involving the same aspects. Internal consistency testing resulted in a Cronbach's alpha of 0.56 in the 12 items. 8 more items were added in the last round of the Delphi study for a new evaluation. After the reevaluation, an acceptable Cronbach's alpha of 0.85 was obtained. The questionnaire showed three factors, the first being physical fatigue, then second with psychological fatigue and the third factor being emotional.
ConclusionThe developed questionnaire is short, simple and easy to apply; it is clear and concise to evaluate the perception of fatigue in women during labor, showing adequate content, internal consistency and face validity.
Fatigue is a symptom commonly reported by pregnant women as part of the childbirth experience. It might have a negative effect on the health of both mother and fetus, being strongly related with anxiety and labor pain.1 Fatigue can change the uterine contraction pattern with consequent increase of the first stage of labor.2 Research has been showing that fatigue can also adversely affect the fetal heart rate and produce fetal distress, increasing the incidence of instrumental and cesarean births. In addition, fatigue may be associated with a decrease in the mother's interest in the newborns, “baby blues” and postpartum depression, compromising the mother–baby bond.2–6
Therefore, its of great importance that physical therapists who provide childbirth care evaluate fatigue, since the increase of fatigue can negatively affect the tolerance to pain and the efficacy of pull, reducing the mother satisfaction. As consequence, tired mothers choose to have a cesarean section.5–7 Attempts to measure the nature, severity and repercussions of fatigue during childbirth led to the use of several instruments, including the Visual Analogue Scale (VAS),1,2,7,8 the Modified Fatigue Symptom Checklist (MFSC)9,10 and the Fatigue Scale.3 None of them, however, was developed to study fatigue in the childbirth environment, disregarding the physical, emotional and cultural characteristics involved in that moment.2,3,7–11
The multiple dimensions (biological, psychological, social and cultural) of fatigue experienced by women during labor requires the development of an instrument capable of properly reflecting that construct, so that the obtained results are not inaccurate nor spurious. Therefore, the objective of this study was to develop and validate a questionnaire capable of identifying the maternal perception of fatigue during labor.
MethodThis study developed a health status measurement instrument in three phases (Fig. 1). For the purposes of this study, fatigue was defined as an unpleasant sensation, associated with tiredness that involves physical, psychological, and emotional symptoms that are not relieved by rest and interfere with the ability to perform usual activities.12
Phase 1 – Developing of the first version of MCFQThe first phase consisted in the creation of a conceptual map to assemble the initial version of a questionnaire. An extensive literature search through various databases such as MEDLINE, LILACS, SciELO, Web of Science and CINAHL, without language or date restrictions, was carried out to seek scientific findings about the evaluation of maternal fatigue associated with labor. We selected the main clinically relevant signs and symptoms evaluated in these studies.
Input for the questionnaire also included statements relating to maternal fatigue, obtained from semi-structured interviews of postpartum woman and healthcare providers that have worked directly with women during childbirth. Those interviewed were volunteers and signed an informed consent form. All interviews were conducted by a single researcher, and were recorded with a mobile device S4 mini, Samsung brand, and later transcribed for analysis and selection of items that would be included in the first version of the questionnaire.
Both groups – mothers and health professionals – were not informed about the concept of fatigue used as reference for the research, in order not to influence the responses of the volunteers. This was because, at this stage, we sought to indirectly recognize the perception of fatigue by health professionals and mothers, as well as to identify which signs and symptoms were recognized by them as being related to fatigue.
The qualitative content was used to facilitate understanding of the object of study (maternal fatigue in childbirth). All the signs and symptoms described by the postpartum women and health professionals were grouped until they realized they were repeating themselves (saturation method).
Various factors were used as eligibility criteria for the interviewed healthcare providers. Those interviewed were obstetricians, obstetrical nurses, or physical therapists with a minimum of three years experience in the delivery room. The criteria for postpartum women to be interviewed was to have experienced labor at the most within 10 days.
Phase2 – Developing consensus on the MCFQUsing the theoretical basis of the literature and the interview results, we created the first version of the questionnaire, which was submitted to three rounds of a Delphi study. This second phase aimed to reach consensus among experts about the items that would compose the MCFQ.
Professionals in the field were invited to participate in the panel of experts via e-mail and had to explicitly express their interest in participating. Upon confirmation from the participants, the initial version of the questionnaire was delivered through an email attachment of a “Google Docs” link that led to the form corresponding to the first round of the Delphi study.
At this second stage for the Delphi study, we considered the following eligibility criteria: professionals in medicine, nursing, physical therapy and doulas that assist women giving birth, with a minimum experience of 10 years in the delivery room. The group of experts also needed to come from different regions of Brazil.
On the forms sent in each round of the Delphi study, for each item there were five options: “strongly agree,” “somewhat agree,” “neither agree nor disagree”, “somewhat disagree,” “strongly disagree”. The participants could choose only one of the options, demonstrating their level of agreement with the continuity of each item in MCFQ.
For response analysis, a consensus/agreement criterion was established when 80% or more of the experts choose “strongly agree” or “somewhat agree” on a Likert scale for each item of the Delphi list.13–15 The items that obtained consensus level below 50% were promptly eliminated. When an item had a degree of agreement between 50% and 79% it was put up for discussion in the following round. If a consensus of 80% was reached by the group, the ratification of that item would take place in the following round. Suggestions by the collaborators for the composition of the questionnaire were also included.
Responses from the first round were analyzed to determine the level of consensus, identifying the overall trend of the answers. This information was added to the group's views and compiled in the form of a report sent to all participants, so they could be examined by each member individually. Their identification was kept confidential, ensuring anonymity.
Simultaneously with the submission of the report, a link was sent to each member of the experts group, which redirected to the second-round questionnaire, requesting the submission of new responses. This version of the questionnaire was developed based on the answers from the previous version, including and excluding items according to the experts’ opinion. After analysis by the experts, a condensed third version of the questionnaire was developed and sent along with their respective report. Furthermore, in the third round, experts were asked to include their opinion in the questionnaire answer options. One format consisted of three options (none, a little, a lot) and the other format included five options (not a bit, a little, more or less, a lot, extremely). It was necessary for more than half of the experts to recommend the same format to confirm that questionnaire answer option. The instrument was then evaluated by 10 postpartum women about its clarity and coherence of the items.
Phase 3 – Analysis of measurement properties and exploratory factorial analysis of the MCFQThe third phase consisted of instrument validation, following the recommendations of the Consensus-based Standards for the selection of health Measurement INstruments (COSMIN) and Terwee et al.13 An Exploratory Factorial Analysis (EFA) was also performed to identify latent components and reduce items.
The verification of the transformation of the items into a scale occurred as part of a pilot study, composed of 30 women during the active stage of labor. This stage ends the face validation. The Cronbach's alpha values found, between 0.70 and 0.95, were acceptable. In this step the questionnaire items were verified to see if they were clearly and unequivocally understood by the target audience, this way concluding the face validation.
The MDFQ was then applied by adequately trained researchers in a sample consisting of 10 women in labor for each item of the questionnaire. As it had 20 items, the final sample consisted of 200 parturients, this way evaluating internal consistency and EFA.13
Inclusion criteria for this study were pregnant women aged 19–35 years, primiparous or multiparous, and in the active stage of labor. Active labor was characterized as cervical-uterine dilation equal or higher than 4cm and uterine activity with contractions equal to or higher than 3 contractions in 10min, being them strong, rhythmic and lasting more than 30s.16 Women in the second stage of labor were excluded.
The women during childbirth were invited to participate in this study, and after receiving explanations about the objectives and procedures of this research, signed the consent. An evaluation form was then applied to acquire socioeconomic, clinical and labor characteristics data.
Sample characterization was done through descriptive statistics and data was displayed in frequency distribution tables for the categorical variables, and measures of central tendency and dispersion for the numerical variables. Internal consistency for the instrument was calculated through Cronbach's alpha, with values between 0.70 and 0.95 considered acceptable.13
The Kaiser–Meyer–Olkin (KMO) test for sampling adequacy was calculated to verify if the questionnaire had factorability. Then, the EFA was performed to verify the number of factors through a Cattel Scree Test Plot14 and the definition of erratic items, revising and excluding those below the 0.3 threshold in all factors. The evaluation of the multidimensionality of the instrument was carried out by the analysis of the main component using the Varimax rotation method with the Kaiser normalization.
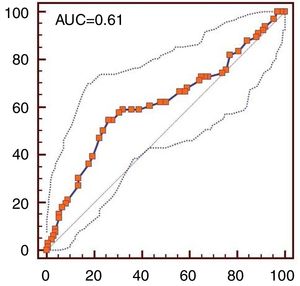
To categorize maternal fatigue through a cut point, a Receiver Operating Characteristic Curve (ROC) curve accuracy evaluation was done, defining the sensitivity, specificity, area below curve (AUC) and confidence interval of 95% (IC95%). The reference standard used in the categorization of MDFQ fatigue was the Visual Analogic Scale (VAS). This scale varies in discrete numbers from one to ten, with reference values from one to five (low fatigue) and six to ten (high fatigue).2
This study was approved by the Research Ethics Committee of the Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil (Protocol Number: 1.903.925).
ResultsPhase 1 – Developing of the first version of MCFQAfter the literature review and the interviews with mothers and health professionals were done, the conceptual map that guided the construct about maternal fatigue during labor was created (Fig. 2). The first version was composed of 51 questions involving physical, emotional and cognitive aspects based on the literature and interviews. Seven healthcare professionals from public hospitals in northeastern Brazil contributed in this phase. They were obstetricians (57.14%) or nurses (42.86%), female (85.71%) or male (14.28%), 41.57±12.23 years old, 13.42±14.16 years of experience, with specialization (85.71%) or Masters’ degree (14.28%). Seven postpartum women from a public hospital, who underwent vaginal delivery also contributed to this version. They were 26±7.92 years old, primiparous (71.43%) and multiparous (28.57%).
In an attempt to not influence the volunteers’ responses, both postpartum women and healthcare professionals were unaware of the fatigue concept used as referenced in this phase of the research. This was necessary since at this phase we intended to identify what the healthcare professionals and patients understood about maternal fatigue as well as what signs and symptoms were recognized by them as being related to fatigue. Later during the Delphi study, the fatigue concept used as referenced in this study was revealed to the experts for them to be able to identify in the questionnaire the items that were most appropriate in revealing that concept of fatigue.
Phase2 – Developing consensus on the MCFQThe first version of the questionnaire was submitted to a Delphi study. For this second phase of the study, 43 healthcare professionals who were experts in the field were contacted by e-mail and asked to be part of the expert panel that would analyze the questionnaire. Only 26 healthcare professionals responded, one did not agree to compose the expert panel, and two others did not meet the pre-established eligibility criteria, “time experience working with parturient women”. Therefore, the initial sample of experts consisted of 23 professionals.
Delphi study was composed of three rounds. The first round was completed by 14 out of the initial 23 volunteers that composed the expert panel. There was a 39% loss of the original panel. The second round was composed of 14 members and there was a 100% retention after this round. The third round was composed of 14 experts and 13 responded to this last round (7.14% sample loss). The volunteers excluded from the analyses had not sent us the Delphi list on time.
About the number of issues that composed the MCFQ instrument, in each phase of the Delphi Study it was observed that after the first-round analysis, 49 items from the first version remained in the questionnaire for the second round. Two questions were summarily excluded because they fell below the minimum threshold of 50% of consensus to remain in next phase. Furthermore, five additional questions were included by participants’ suggestion, resulting in a questionnaire with 54 items that composed the second round. Those questions focused exclusively on the analysis of their content.
After the analysis of the second round of the Delphi study, the questionnaire was significantly reduced. Thirty-one items were eliminated due to lack of the previously established 80% consensus and lack of suggestions for changes or indication of discussions about the items. The third version of the questionnaire, resulting from the second round, was composed of ten questions. These ten items had obtained consensus during the previous round after ratification by the experts. Twelve separate items were placed for debate and two new additional questions were suggested by the group. At this point the questionnaire resulted in 24 total items, 10 with a final consensus and 14 for discussion in the third and final round.
Upon completing the third round in the Delphi study only 2 out of the 14 questions that had been opened for discussion reached a consensus level (84.6% and 92.3%). These two items were added to the 10 questions from the previous round and remained in the final version of the questionnaire. Regarding the questionnaire response options, 69.2% of the expert panel recommended to assess the responses with five options. These options ranged from 1 (not a bit) to 5 (extremely) on a Likert scale. Thus, the final questionnaire that underwent evaluation by parturient women in the pilot study consisted of 12 questions total.
The 10 pregnant women in labor found it difficult to answer two of the items, considering them too long for the moment they were experiencing, so they were modified to come into line with the needs suggested by them.
Phase3 – Analysis of measurement properties and exploratory factorial analysis of the MCFQFace validity was carried out through two pilot studies for transforming two items into a scale. The first, consisting of 30 pregnant women during labor (5.8±1.67cm of uterine cervix dilatation) showed a Cronbach's alpha of 0.56 for the 12 items of the MCFQ from the latest version of the Delphi study (Table 1). This result is considered inadequate for a transformation into scale, because it did not present an acceptable value of Cronbach alpha between 0.70 and 0.95. Therefore, a second pilot study with 30 more women was carried out (5.6±1.43cm of uterine cervix dilatation).
Eight items from the Delphi study were added to this second pilot study, as they were considered relevant by the researchers, because they represented the conceptual map created for the identification of the maternal fatigue construct, for the items to become a scale. Cronbach's Alpha for the second pilot study with the new included items was 0.85, therefore acceptable for the transformation into a scale, which contained 20 items (Table 1).
After the finalization of face validation, the questionnaire was applied in 200 women during labor for internal consistency and factorial analysis. Mean age for the women was 24.61 years (SD=6.21) and gestational age was 39.18 weeks (SD=1.14). Most of them had 5–7cm of uterine dilation and were in their first experience of delivery (40.0%).
Internal consistency of the questionnaire was composed of a Cronbach's alpha of 0.84 in the 200 parturient. However, negative correlation and values below 0.3 were seen in 5 items, which were excluded, two items being excluded from the latest version of Delphi and three of the new items included by the researchers (Table 1). After the evaluation of the internal consistency, the final version of the MCFQ resulted in 15 items (Appendix 1).
KMO sample adequacy measure value found was 0.590, indicating sufficient correlations between the variables for carrying out an exploratory factor analysis.15 The analysis of the main component by the Varimax rotation method with Kaiser normalization verified that the questionnaire is multidimensional, with three factors best represent its composition.
Table 2 shows the distribution of the factorial loads of all the items in the MCFQ. The first factor consists of nine items with the semantical content that expresses physical fatigue, extreme tiredness or exhaustion. The second factor, with three items reflecting the contents of psychological fatigue, with feelings of fear and concentration deficit/attention. The third factor, consisting of three items, with contents of emotional fatigue, with feelings of incapacity, anguish and irritation.
Factor analysis of the three factors of the MCFQ.
| Items | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| 1-Você está se sentindo cansada? | 0.676 | −0.55 | −0.87 |
| 2-A dor está te impedindo de ajudar no trabalho de parto? | 0.422 | −0.79 | −0.23 |
| 3-Você está com sono, com os olhos pesados? | 0.436 | 0.27 | −0.57 |
| 4-Você está conseguindo descansar entre as contrações? | 0.356 | 0.19 | 0.22 |
| 5-Você consegue realizar atividades como mudar de posição, caminhar, ficar de cócoras ou tomar banho? | 0.457 | −0.78 | −0.43 |
| 6-Você está sentindo o corpo ou as pernas tremendo? | 0.532 | −0.61 | −0.44 |
| 7-Você está com medo? | 0.22 | 0.487 | −0.43 |
| 8-Você consegue prestar atenção no que as pessoas falam a sua volta? | −0.54 | 0.312 | 0.29 |
| 9-Está difícil entender e seguir as orientações que você está recebendo? | −0.94 | 0.452 | −0.51 |
| 10-Você está se sentindo sem energia? | 0.511 | 0.17 | −0.42 |
| 11-Você está sentindo necessidade de descansar? | 0.375 | −0.91 | −0.47 |
| 12-Você está se sentindo fraca? | 0.491 | 0.25 | −0.91 |
| 13-Você acha que precisa de ajuda para parir? | −0.74 | −0.53 | 0.365 |
| 14-Você está sentindo angustiada? | 0.15 | 0.21 | 0.476 |
| 15-Você está se sentindo desanimada, impaciente ou irritada? | −0.63 | −0.71 | 0.582 |
The proposed cut-point and ROC curve indicators for categorization of the fatigue level are described in Fig. 3. The cut point that best discriminated the fatigue level was represented by scores above 50 points (AUC=0.61; IC95%=0.54–0.68; p=0.011), indicating moderate sensitivity (value=54.5; IC95%=41.8–66.9) and specificity values (value=73.8; IC95%=65.6–81.1). Therefore, the questionnaire was categorized into: low fatigue (scores lower than 50 points) and high fatigue (higher than 50 points).
DiscussionThis study resulted in the development and validation of an instrument to assess maternal perception of fatigue during labor: The Maternal Perception of Childbirth Fatigue Questionnaire (MCFQ). The final version of the questionnaire was composed of 15 items, with an estimated application time of 5min. Each item has a 5-point Likert scale that can be categorized as low fatigue (15–50 points) and high fatigue (51–75 points). In addition, the MCFQ showed good internal consistency, what represents the construct evaluated through the conceptual map, also demonstrating three factors. To the best of our knowledge this is the first questionnaire developed for the specific purpose of assessing fatigue during labor and childbirth.
In its conception, the MCFQ considered the perspective of postpartum women in addition to the viewpoint of healthcare professionals from different areas in the field. These perspectives confirmed and strengthened the relevance of the patients as experts in their personal health experience.16,17 This is an important feature of patient-centered health care practices, in line with current trend, as the patient has an increasingly active role in decision-making regarding their own health treatment.18,19
Rigorous psychometric testing was carried out to ensure validity and reliability. Internal consistency and face validity of the MCFQ resulted in an above acceptable Cronbach's alpha, for this kind of scale.13 It is of note that the application of the MCFQ occurred in the form of an interview and the favorable internal consistency results obtained indicate that this is a suitable way of applying the questionnaire.
In the factor analysis the MCFQ represented three factors: one related to physical fatigue; other to psychological fatigue and the third was related to emotional fatigue. Since childbirth is an event requiring high energy expenditure due to an association of uterine contractions with feelings of anxiety, concern and fear,1–5 it was already expected that these three types of fatigue were associated, corroborating the conceptual map created for this construct. The term physical fatigue is used to describe a decrease in physical performance associated with an increase in difficulty in performing a task or exercise,20 while psychological fatigue is associated with attrition related to decreased motivation21 and emotional fatigue to an intense exhaustion, which results in the lack of will and willingness to perform the activities.22
This instrument will help the decision-making of physical therapists and will guide the childbirth assistance. The advances with the use of this kind of instrument can also impact directly the development of new physical therapy techniques to reduce those symptoms during labor, to review procedures, and to monitor the existing protocols, influencing positively the women's health.
This study has the following limitations: it was not possible to evaluate criterion validity, as there is no gold standard instrument to measure fatigue during labor. Because it is an event with reduced length and that in general needs little intervention, it was not possible to perform a reliability analysis by inter-rater and intra-rater test–retest.
The MCFQ was clearly understood by the target audience, showing both good face and content validity and being concise and relevant. The questionnaire has adequate measurement properties, being established as an adequate instrument to evaluating the clinical perception of maternal fatigue during labor, also presenting three factors, one related with physical fatigue and the other two with psychological and emotional fatigue.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.
This paper is part of a Special Issue on Women's Health Physical Therapy.