Pain experience has a multidimensional nature. Assessment and treatment recommendations for pain conditions suggest clinicians use biopsychosocial approaches to treat pain and disability. The current pain research is overwhelmingly skewed towards the study of biological and psychological factors including interventions, whereas, cultural factors are often ignored.
ObjectiveThe aims of this Masterclass is threefold: (1) to discuss cultural influences on pain, (2) to provide strategies for delivering appropriate pain education and exercises in culturally diverse people with chronic pain, and (3) to present challenges and future directions to clinicians and researchers.
DiscussionCultural factors have a relevant influence on the way individuals experience and manage health and illness. Thus, people with different cultural experience perceive, respond, communicate and manage their pain in different ways. In this aspect, the contents of pain education should be presented using different culturally appropriate examples, metaphors, images, and delivery methods that may enhance the impact of the message. Efforts should be made to produce and spread culturally adapted evidence-based materials and resources. In addition, a culturally sensitive approach may help to introduce patients to graded activities, so that they can apply these strategies in culturally acceptable and meaningful ways. Future studies should investigate the effectiveness of culturally-adapted interventions in pain-related outcomes in different pain conditions in patients with different cultural backgrounds.
Chronic musculoskeletal pain is a global health issue.1 Current evidence indicates that pain is modulated by biological, emotional, cognitive, behavioral, environmental, and sociocultural factors.2–4 However, the majority of literature emphasizes the influence of biological and psychological aspects on pain, with the influence of the socio and cultural aspects of pain largely overlooked.5–8
The literature focusing on the influential role of culture on pain has considered variables such as ethnicity, gender, nationality, and language as proxy measures of culture as these variables may reflect cultural differences.9,10 However, according to The United Nations Educational, Scientific and Cultural Organization (UNESCO), culture is defined as “the set of distinctive spiritual, material, intellectual and emotional features of society or a social group, and that it encompasses, in addition to art and literature, lifestyles, ways of living together, value systems, traditions and beliefs”.11 Therefore, an individual can identify themselves as belonging to more than one social group, based on ethnicity, gender, nationality, common interests, or sexual orientation.12 This intersectionality of belonging makes the culture of an individual dynamic and constantly evolving.
Cultural factors have a relevant influence on the way individuals experience and manage health and illness, as well as receptivity to health interventions, their pain behaviors (e.g., coping responses, help seeking behavior), and beliefs (e.g., causes of pain, consequences, how controllable pain is).13 Beliefs, pain-related fear, catastrophizing, and avoidance are key factors in the development of disability in chronic musculoskeletal pain.13,14 Pain catastrophizing, an important component of the fear-avoidance model, has been consistently regarded as one of the most influential determinants of pain-related outcomes.15 The fear-avoidance model suggests that pain may be interpreted as threatening bodily integrity, which may lead to people prioritizing pain control over achieving valued life goals,16 leading to a vicious cycle involving catastrophizing, hypervigilance, and avoidance or escape behavior and, in turn, leading to disuse, disability, depression and increased pain.16 Although pain catastrophizing can be considered as a maladaptive belief (i.e., negative interpretation about the severity and the concept that unexplained symptoms are usually serious),17 this negative cognitive appraisal can be related to other reasons in different cultures (e.g., the feeling of abandonment by God during their suffering).18
Although some attempts have been made to explore the influence of cultural factors on pain, pain catastrophizing, beliefs, and coping strategies, it remains challenging for clinicians to use this information in their practice.19 For instance, while clinical practice guidelines recommend addressing misconceptions about pain as one of the first line of interventions in patients with musculoskeletal pain,20 the implementation of such interventions in culturally and linguistically diverse communities remain challenging in clinical practice.21 Given these considerations, the aims of this Masterclass are: (i) to discuss cultural influences on pain, pain catastrophizing, pain beliefs and behavior, (ii) to provide strategies to deliver pain education and exercises in culturally diverse people with chronic musculoskeletal pain, and (iii) to present challenges and future directions to clinicians and researchers about culture and pain.
How can culture influence pain, beliefs, and pain catastrophizing?The literature highlights the role of race/ethnicity22,23 and sex/gender24 differences in pain prevalence, coping, sensitivity, and tolerance. For example, African Americans, Asians, and Hispanics experience and report more intense pain compared to their non-Hispanic White counterparts.23 Despite this, African Americans and other ethnic minorities receive lesser and poorer care for their pain.25 Sex/gender differences can also be related to cultural factors. In some cultures, boys and men are taught to tolerate pain, and endure painful experiences, while girls and women are taught to be sensitive, careful, and to verbalize discomfort.26
Cultural variability in beliefs regarding the causes and consequences of pain play a significant role in the patient's pain experience.13,27 For example, in Mexican-American culture, pain can be viewed as being due to God's will, punishment or penance.27 The Aboriginal Australians with chronic low back pain did not express their pain and demonstrated few pain behaviors because of cultural beliefs that pain is a social and spiritual dysfunction.28 In Zulu culture, pain may be considered a consequence of bewitching.29 Family beliefs (e.g., enduring pain, the role of folk healers), spirituality, and religiosity30 are suggested to play a role in how pain is expressed and managed in Hispanic cultures.31 In case of beliefs emphasizing supernatural or divine causes of pain, the external locus of control can be associated with increased pain intensity.32
Evidence suggests that cultural beliefs can be changed following healthcare interactions.33 For example, people from rural Nepal tend to perceive back pain as a “normal” part of aging and they do not seek care;34,35 whereas, back pain is considered a biological phenomenon in urban Nepal,36 resulting in greater healthcare utilization. Aboriginal Australians with chronic low back pain presented negative beliefs and misconceptions about their condition among those who were exposed to healthcare interactions.33 The influence of the dominant health approach in Western societies appeared to contribute to unhelpful pain beliefs as an example of acculturation (i.e., a process by which individuals adopt beliefs and behaviours of another dominant culture).33
People with different cultural experience perceive, respond, communicate and manage their pain in different ways.27 In Western society, people with chronic pain may experience shame, embarrassment, and humiliation as a consequence of pain-related disability.37 Sharma et al.19 compared pain-related beliefs and catastrophizing across countries, language groups, and country economy. The authors found that pain-related beliefs were different in between-country and between–economic region comparison. However, there were no difference in pain beliefs in people living in the same country but speaking different languages. Pain catastrophizing was greater in people with chronic pain from the United States than Portugal, and people from Australia presented more pain catastrophizing than samples from Denmark and Brazil. The interactions between pain catastrophizing, pain sensitivity, and culture/ethnicity should also be considered. Fabian et al.38 found that only situational catastrophizing varied by ethnicity, with African Americans reporting greater catastrophizing than Asian/Pacific Islanders and Caucasians. The authors found that situational catastrophizing significantly mediated pain intensity. Another study found that pain catastrophizing partially mediated race differences in pain tolerance and mediated sex differences in pain intensity.39
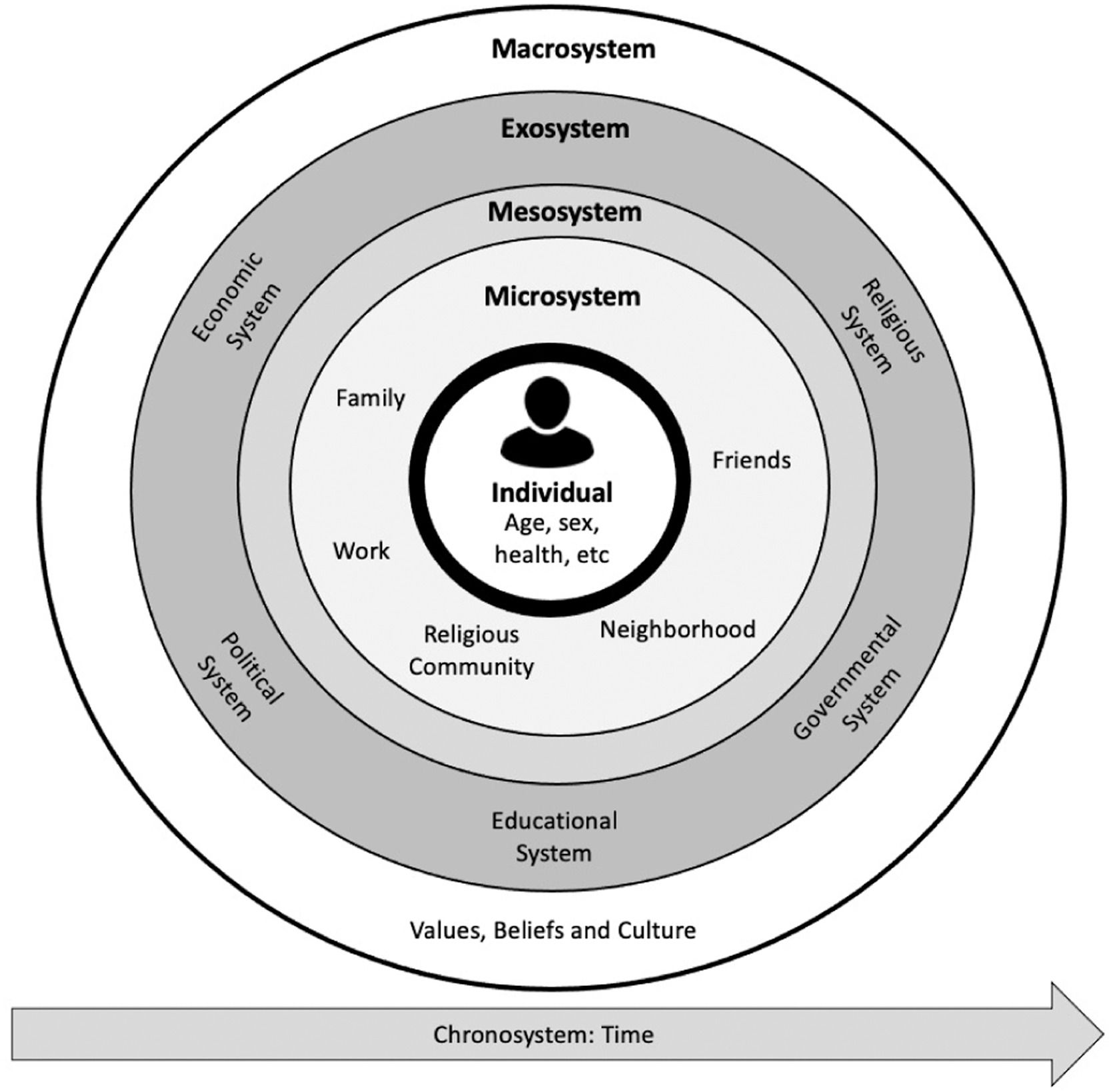
Culture and the dynamic biopsychosocial modelThe biopsychosocial model, that is well endorsed in the pain field, supports the notion that biological, psychological, societal, and lifestyle factors are interconnected and mutually reinforcing.40 This model has been criticized because it has been often applied in a fragmented manner in clinical practice and research.6–8 The narrow focus on some psychological dimensions (e.g., behavior and cognition) and minimal consideration of the social dimensions (including culture) perpetuate a reductionist view of the pain experience.6,7 It is important to highlight that the influence of bio, psycho and social dimensions on health are not fixed, but rather interact with each other over time.41 Lehman et al.41 proposed that the biopsychosocial model should be viewed as a dynamic model of health constructed as a product of the reciprocal influences of biological, psychological, interpersonal, and macrosystem contextual dynamics that unfold over personal and historical time. This model considers interpersonal dynamics over the life span including direct contact with others, as well as the reverberating consequences of others' actions. The interpersonal dynamics of health can be explained using Bronfenbrenner's ecological framework and concepts of microsystem, mesosystem, exosystem, and macrosystem factors (Fig. 1). The microsystem factors include family members, work environments, peers, and community health resources. The mesosystem relies on interactions among various microsystem factors (e.g. multiple family members and social groups). The exosystem refers to an indirect influence when the microsystem is affected by dynamics within their own microsystems (e.g. influence from spouses' employment setting). The macrosystem (referenced as contextual dynamics) includes shared culture, norms, policies, and values.
Clinicians should be mindful that all biological, psychological, and social factors may occur within contextual dynamics and are influenced by culture. Thus, we suggest that during the biopsychosocial assessment of patients with chronic musculoskeletal pain, clinicians should use open and reflective questions to capture patients’ pain experience, pain beliefs, and coping strategies.4 Further, clinicians should avoid making stereotypical cultural judgments based on cultural affiliations. Clinicians should be respectful, open, empathetic, authentic, sensitive, and caring throughout their clinical encounter. Therefore, the concept of a non-judgmental patient-centered view should be cultivated and derogatory labels (both with colleagues and patients), such as “catastrophizer”, “avoider”, or “malingerer” should be avoided.42Box 1 provides example questions that clinicians can use to obtain a culturally sensitive pain assessment.
Examples of questions to address pain beliefs.
Although several interventions [e.g. cognitive functional therapy,43,44 group cognitive behavioral treatment,45 acceptance and commitment therapy, cognitive behavioral therapy,46 mindfulness,47 multimodal treatment48], have been described to address maladaptive pain beliefs, pain catastrophizing, fear of movement, pain intensity, and disability, this paper focuses on treatment approaches such as pain neuroscience education (PNE),49 cognition-targeted exercise therapy,50 behavioral graded activity,51 and graded exposure.52
Pain neuroscience education (PNE)PNE aims to decrease the perceived threatening nature of the patients’ pain to facilitate engagement with physical activities which specifically target beliefs, pain-related fear, pain catastrophizing, and avoidance. The current evidence suggests that PNE can be effective for several pain-related outcomes including pain intensity, disability, pain catastrophizing, and kinesiophobia in the short- to medium-term in patients with chronic musculoskeletal pain.53 The impact of PNE on patients’ cognition and fear-avoidance beliefs is limited to small to medium effect sizes,53 illustrating that more is needed than education alone. A recent review showed positive results in favor of the addition of PNE to physical therapy treatment on disability and pain intensity in patients with chronic low back pain.54
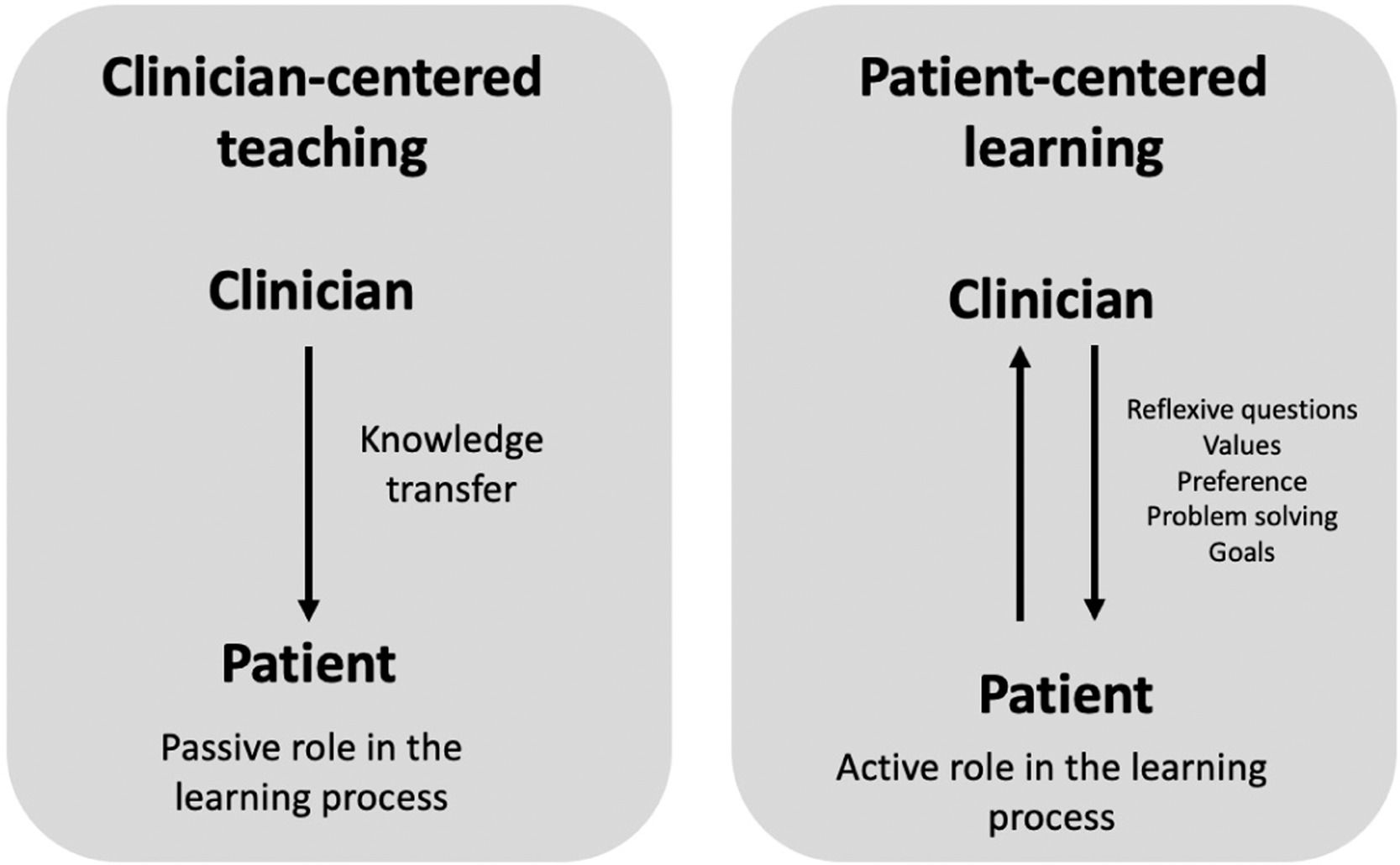
Patients want to receive a clear and consistent message about their pain, treatment options, and self-management strategies.55 A culturally sensitive PNE session should take into account that patients have an expectation that the provider will be a good communicator and will listen to concerns, recognizing the legitimacy of their pain, and respect their culture, values, and preference. The focus of a PNE session should switch from “clinician-centered teaching” to “patient-centered learning.” Hence, clinicians should avoid imposing their knowledge about pain biology over patients’ concepts, values, and beliefs. During a clinical encounter, clinicians should use open-ended questions to capture the patients’ beliefs about their pain. This strategy provides insight into the patient's cultural meaning of pain, beliefs, and coping strategies. Within the context of “patient-centered learning,” it is expected that clinician and patient build a two-way street for interaction (Fig. 2).
A culturally sensitive PNE session is important because patients present different explanations for their pain. For example, people from rural communities in Nepal have contrasting beliefs about pain ranging from "pain as a normal part of life or aging and that they should live with it" to "pain is a result of bad deeds from the past lives or a result of black magic".34 Some Brazilians can consider their pain as a loss of faith or even a punishment from God leading them to seek prayers and rituals to receive forgiveness. In some South African cultures, pain may be interpreted as a punishment from ancestors. Thus, it is important to consider that the same set of target key PNE concepts may not necessarily work in all cultural groups. Clinicians need to identify key educational concepts in a pain education program that may help to produce a more focused, culturally appropriate, and succinct program.
Clinicians should consider several audiovisual aids to deliver PNE. While slide presentations work for western cultures, they did not seem to work in the context of Nepal as patients had no previous experience with this approach. Printed postcards appeared to be a good alternative in the Nepali context.36 In a South African context, printed materials which patients can take home and share with friends and family are regarded as valuable and may enhance the impact of the message.56
Clinicians should acknowledge, respect, and validate rather than confront patients’ beliefs and cultural values. It is helpful for patients if clinicians respect their beliefs but offer alternative explanations and draw patients to reflect on their pain problems and explain contributors to pain such as sleep, activity levels, stress, and mood. These are often effective if patients or their family members can draw examples from their own experiences. If not, other examples from local context may be used here to demonstrate these relationships. In Box 2 we present some examples of metaphors adapted for South African to explain pain concepts.
Pain education messages adapted for South Africa as an example that pain education concepts should be adapted considering the patients’ context and cultural background.
A culturally sensitive PNE approach may help introduce patients to graded activities (i.e., behavioral graded activity, graded exercise therapy, graded exposure in vivo, or cognition-targeted exercise therapy), so that patients can apply these strategies in culturally acceptable and meaningful ways. Moreover, without applying the knowledge regarding pain into daily life, deep learning and long-term effects cannot be expected.
The available evidence suggests that patients with chronic spinal pain who have received PNE (implying that patients have increased their understanding of their pain problems, and the threatening nature of pain [flares] is reduced), respond better to exercise therapy.57 In line with this, it seems rational that this also accounts for adopting a more active lifestyle,58 but direct evidence supporting this notion is currently lacking. In addition, this is not a linear process, and responses can vary substantially from patient to patient. The synergistic effect of PNE combined with such active approaches was illustrated in a trial with 120 patients with chronic spinal pain randomized to PNE plus cognition-targeted exercise therapy or back/neck school education plus general exercise therapy. The trial found hardly any clinically important changes after the education phase, but medium to large improvements were seen after the cognition-targeted exercise therapy on kinesiophobia and hypervigilance even at 1-year follow-up.57 Both active approaches were associated with marked reductions in pain catastrophizing.57
One key aspect includes changing from the classical symptom-contingent approach (“Stop the activity or exercise once it hurts”) to a time-contingent approach to exercises and daily activities (“Perform the activity or exercise for five minutes, regardless of the pain”). Behavioral graded activity can be used to implement such a time-contingent approach into the patients’ daily life. Behavioral graded activity can be regarded as a culturally sensitive approach as it is a behavioral treatment integrating the concept of operant conditioning to increase the level of physical activity in the patient's daily life.59 Behavioral graded activity is an effective approach for patients with chronic low back pain60 and osteoarthritis.59
For addressing maladaptive beliefs and pain catastrophizing, especially for highly feared activities and exercises, other approaches are needed. Approaches that are useful for tackling such highly feared activities include cognition-targeted exercise therapy and graded exposure. The current evidence suggests that cognition-targeted exercise therapy presented superior results over pain-contingent exercise therapy in patients with chronic low back pain.57 Limited evidence suggests that graded exposure is more effective than behavioral graded activity for improving disability and catastrophizing at short term in patients with chronic low back pain.60 Graded exposure in vivo is a cognitive behavioral treatment approach that has resulted in positive outcomes in patients with chronic low back pain,61 complex regional pain syndrome,62 whiplash pain,63 and work-related upper limb pain.64 While the evidence favoring behavioral graded activity and cognition-targeted exercise therapy for patients with chronic pain was not generated from different cultural settings, the intervention is considered suitable for cultural adaptation. Future research should examine whether they are generic across cultures.
During cognition-targeted exercise therapy and graded exposure, the therapist continuously assesses, validates, and challenges the patients’ culturally sensitive beliefs about pain and the anticipated outcome of each activity/exercise, to change maladaptive beliefs into positive ones. If certain activities/exercises are too threatening to perform, a preparatory phase of motor imagery can be included (including a home exercise program of motor imagery of the threatening exercise/activity).65 Motor imagery is defined as a dynamic mental process involving the internal representation of an action without its actual motor output.66 Although motor imagery seems to be a promising intervention that could be adapted in different cultural settings, consistent evidence from rigorous studies is still lacking.67 The exercise/activity program should progress towards more feared movements and activities by discussing patients’ fears and maladaptive perceptions, preferentially by asking questions that challenge the patients’ (pain) beliefs. This part of the treatment is highly culturally-sensitive and allows the therapist to adapt to the patient's socio-cultural situation and interpretation of bodily responses to exercises and activities, including pain flares following the threatening exercises/activities. Therapists should try to decrease the anticipated danger (threat level) of the activities/exercises by challenging the nature of, and reasoning behind the patients’ fears, assuring the safety of the activities/exercises, and increasing confidence in a successful accomplishment of the activities/exercise.50 More details regarding this approach, including specific instructions on required communication skills, are described in detail elsewhere.50
Challenges and strategies for cross-cultural pain education and exercisesAmong the many challenges facing healthcare systems, is the major challenge of ensuring effective culturally congruent care (i.e., cultural diversity, sex, race, ethnicity, literacy) and linguistically appropriate information eliminating the disparities experienced by minority groups.68 If cultural factors are not taken into account, the provision of care may be ineffective, if not harmful. Within each cultural group the pain experience includes pain expression, pain language, cultural context of suffering, traditional healers and lay remedies for pain, social roles/expectations, and perceptions of the health care system. Therefore, efforts should be made to produce and spread culturally adapted evidence-based materials and resources including language, content, and images that would resonate with the target population.69–72
Communication to the public aiming to improve knowledge and modify beliefs and attitudes about pain in multicountry public awareness campaigns (e.g., sponsored by Organizations) seems logical. However, the advantage associated with uniformity of practices and messages across countries is ambiguous, as it shows consistent global messages but limited adaptation to local situations.
During clinical practice, providing culturally appropriate services is, in many ways, more difficult because it may require clinicians adapting therapeutic interventions to their culturally diverse patients.73 There are still some concerns if cultural adaptation models that typically aim to adapt an intervention for one or more diverse groups in a way that retains fidelity to the core components or the original intervention should be used.72,74 For example, researchers in the area of low back pain have identified 30 key messages that are important to deliver to patients with low back pain based on experts’ and patients’ perspectives.75 However, it is unclear which of these target key messages produce clinically meaningful changes in pain and physical function or produce behavioral modifications to generate these changes.
Clinicians should be aware of patients’ needs and goals and how cultural factors can shape patients’ perceptions, conceptions, and unhelpful beliefs about exercises (e.g., fear of injury, negative consequences). For instance, adherence to exercises can be influenced by firm rules and norms about gender roles in some cultures (e.g., women are responsible for household duties, exercise is regarded as a ‘masculine’ and inappropriate practice for women)76 and also by psychological barriers such as depression (e.g., post-war trauma).77 Clinicians may have difficulties in challenging unhelpful beliefs, enhancing self-efficacy, providing safety-cues, providing advice on suitable levels of pain, and providing advice on exercise modification where language difference is an issue. In these cases, a peer-led exercise and education program can be effectively utilized to overcome language and cultural barriers, to alleviate pressurized health care professionals, and to facilitate behavior change.56,78 Another aspect to be considered is that some patients require privacy to do exercises, while others prefer to engage in group exercise sessions composed of individuals of the same community where they feel safe and accepted.79 Strategies for the development of culturally adapted educational and exercise interventions are presented in the Supplementary Material.
Future directionsCross-cultural adaptations (i.e., linguistically appropriate and culturally sensitive) are necessary before using these interventions in a population which is different from the one used to develop the intervention. Clinicians should be trained to deliver a culturally sensitive approach in their practice and programs developed for minority groups might help to decrease health inequalities. Currently, few studies have investigated the feasibility36,80 and effectiveness of a culturally-sensitive pain education intervention in patients with (persistent) pain.72 Further research, especially including non-Western populations and minority groups (e.g., migrants and refugees), are essential to determine the extent to which pain treatments may need to be culturally adapted to make them most appropriate to new populations who may live in different countries or speak different languages than those for whom the interventions were first developed. In addition to the growing concerns about evidence-based interventions in the pain field, attention to cultural diversity is crucial and should start in the entry-level physical therapy program. It would be valuable to integrate students and community members from a variety of ethnocultural backgrounds, embracing the diversity in the classroom to provide opportunities for experiential learning.12
ConclusionMaladaptive pain beliefs and behaviors can be shaped by patients’ culture. Clinicians should consider patients’ beliefs, values, and practices to provide individualized care to their culturally diverse patients. In this aspect, the contents of pain education should be presented using different culturally appropriate examples, metaphors, images, and delivery methods that may enhance the impact of the message. A culturally sensitive approach may help to introduce patients to graded activities, so that they can apply these strategies in culturally acceptable and meaningful ways. Future studies should investigate the effectiveness of culturally-adapted interventions in pain-related outcomes in different pain conditions in patients with different cultural backgrounds.