The Brazilian Classification of Physical Therapy Diagnosis, developed by the Federal Council of Physiotherapy and Occupational Therapy (COFFITO), has the constitutional objectives of standardizing ethical, scientific and social aspects of the Physical Therapy profession.
ObjectiveTo describe the work process, rationale and proposal for standardization of a physical therapy diagnosis classification system in Brazil.
MethodsA working group was created to propose a standardized classification for the description and codification of physical therapy diagnoses. Some terminologies common to the International Classification of Functioning (ICF) were used to make the nomenclature of diagnoses compatible with the outcomes inherent in the field of physical therapy.
ResultsThe Brazilian Classification of Physical Therapy Diagnosis project culminated in a physical therapy diagnosis model consisting of terms grouped by organic systems and identifying codes. In addition, an application was developed to allow professionals to use the standardized diagnostic classification in an online system.
ConclusionThe diagnostic classification system is expected to advance the Physical Therapy profession allowing the identification of structural and/or functional alterations in a simplified and standardised manner. From a physical therapy perspective, this classification may help to consolidate the autonomy of the Brazilian physical therapists by establishing a clearer pathway between the diagnosis and interventions.
Physical therapy in Brazil ha been recognized and regulated as a higher education profession since 1969 (Decree-Law 938/69, Law 6316/75, COFFITO Resolutions, Decree 9640/84, Law 8856/94).1 The Federal Council of Physiotherapy and Occupational Therapy (Conselho Federal de Fisioterapia e Terapia Ocupacional - COFFITO) is a Federal Autarchy created by Law No. 6316, of December 17, 1975; with constitutional objectives of standardizing and exercising ethical, scientific, and social control of the physical therapy and occupational therapy professions.
Although the definition of the profession in Brazil makes clear the role of the physical therapists in determining a diagnosis of human movement disorders to guide the prescription and application of physical therapy procedures, there is no specific resolution offering guidance about physical therapy diagnoses through a standardized system of classification. The aim of the physical therapy diagnosis classification is to synthesize a health problem or risk of impairments from a functional perspective, to guide the definition of therapeutic objectives, and to monitor the response to interventions.2–5
Despite the International Classification of Functioning, Disability and Health (ICF) being used to describe functional outcomes,6 the ICF was not developed to group the assessment tools used by physical therapists. Although efforts have been made,7–9 there appears to be no standardization of the aspects that should be included in physical therapy diagnoses. A specific classification with a coding system may provide a standardized way for physical therapists to improve diagnostic accuracy and help define physical therapy objectives. Furthermore, this classification can strengthen the professional identity and autonomy, contributing to the clinical reasoning of physical therapists in clinical practice.
Given the lack of a specific classification to provide a physical therapy diagnosis in Brazil, a working group of the COFFITO was created to develop the Brazilian classification of physical therapy diagnosis. In this article, we described the process, rationale, and standardization proposal of the Brazilian Classification of Physical Therapy Diagnosis. The purposes of the Brazilian Classification of Physical Therapy Diagnosis are: (1) to identify and classify the individual's kinetic-functional health condition; (2) to define the therapeutic goal and the respective physical therapy prescription; and (3) to monitor epidemiological data on the individual's clinical-functional evolution.
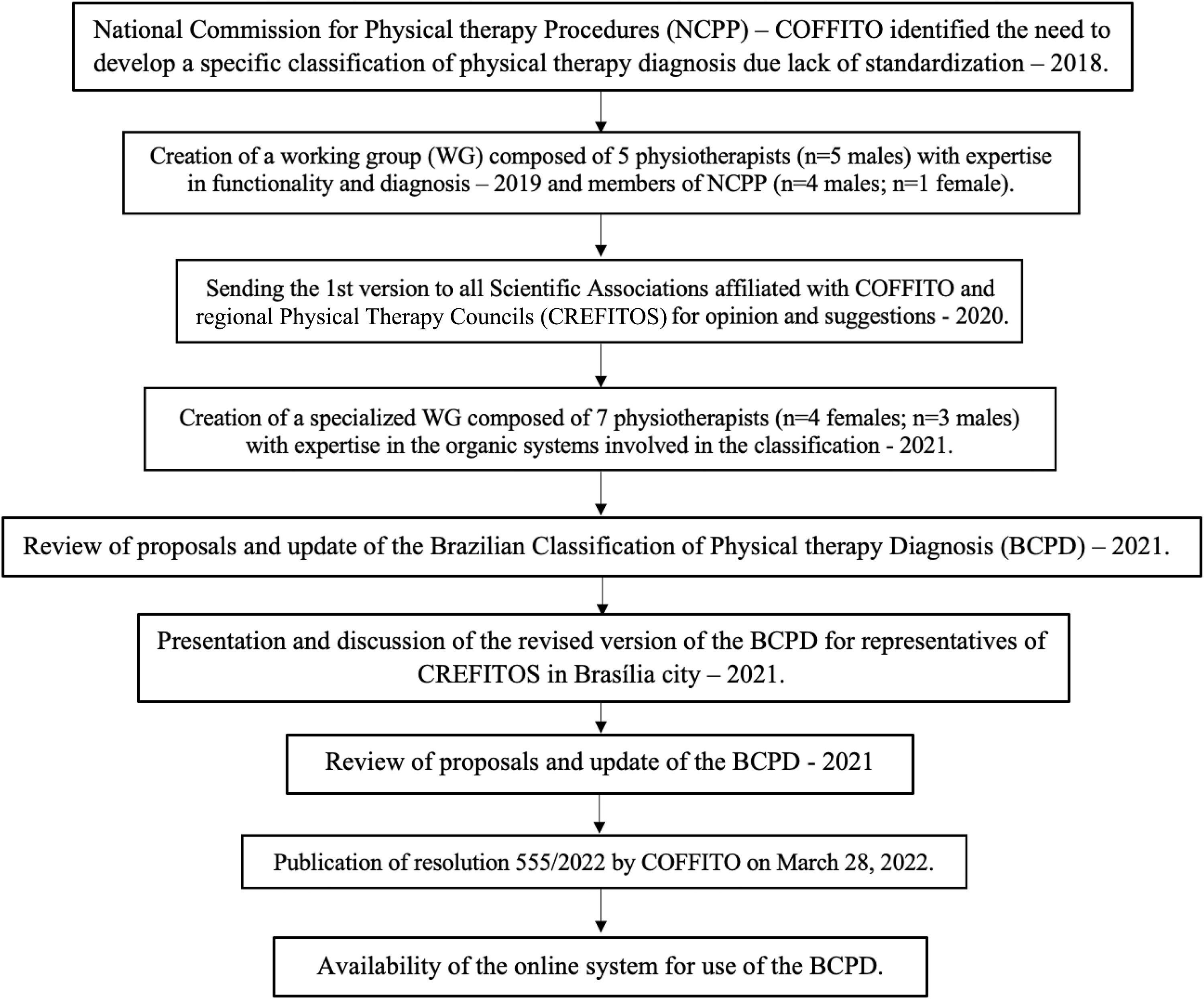
MethodsThe members of the working group were appointed by COFFITO based on the criteria of expertise in the different professional specialties of the organic systems included in the Brazilian Classification of Physical Therapy Diagnosis, and were from different regions of the country, with academic and clinical practice experience. Over a 5 year period, COFFITO hosted face-to-face and online meetings of the working group periodically, totalling more than 30 meetings of about 10 h, totalizing around 300 h. The determination of the variables included in the classification made by the experts was based on the main outcomes related to organic systems. The first version of the classification was published by the COFFITO, following resolution 555/2022 (Fig. 1).10 Furthermore, an online application was developed to enable the use of the classification in an easy, standardized, and free manner for all physical therapists in Brazil. The Brazilian Classification of Physical Therapy Diagnosis can be accessed via the link https://cbdf.coffito.gov.br
Every two years, professionals will be consulted for suggestions and updates will be made as necessary by the COFFITO. The Brazilian Classification of Physical Therapy Diagnosis Commission is continously working to disseminate the classification and to provide training to the professionals in Brazil. The development of part 2 of the classification, which includes the description of changes in patients mobility and social participation, is in progress.
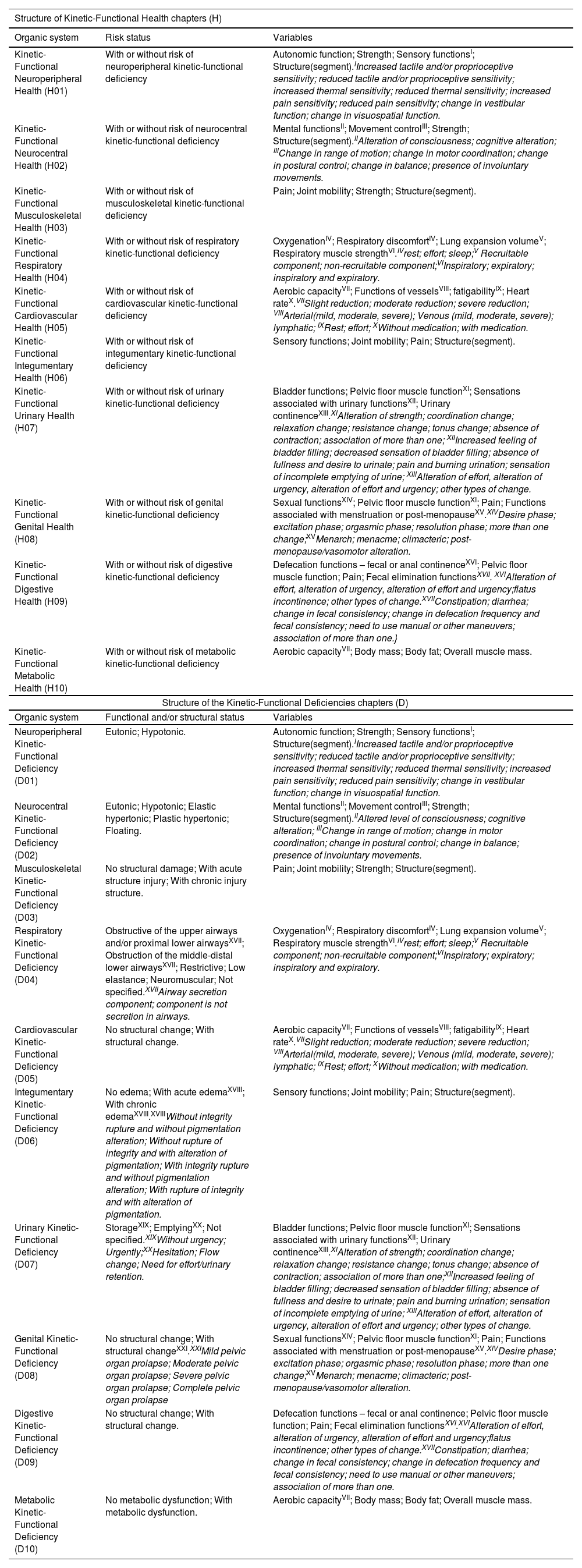
ResultsIn March 2022, a resolution was published by COFFITO establishing the Brazilian Classification of Physical Therapy Diagnosis. In this document, the Brazilian Classification of Physical Therapy Diagnosis based on the domains of body function and structure was detailed, with the physical therapists being able to code physical therapy diagnoses of people with good kinetic-functional health (S), to identify risks of changes in structure and/or function of the body, as well as to diagnose functional-kinetic deficiencies (D), using 10 different characterizers based on body systems, including central and peripheral nervous, musculoskeletal, respiratory, cardiovascular, integumentary, urinary, digestive, genital, and metabolic systems. The description of all variables included in each system is in Table 1.
Description of the structure of the chapters of the Kinetic-Functional Classification related to body structure and function, specifying each system involved and the status and variables measured.
| Structure of Kinetic-Functional Health chapters (H) | ||
|---|---|---|
| Organic system | Risk status | Variables |
| Kinetic-Functional Neuroperipheral Health (H01) | With or without risk of neuroperipheral kinetic-functional deficiency | Autonomic function; Strength; Sensory functionsI; Structure(segment).IIncreased tactile and/or proprioceptive sensitivity; reduced tactile and/or proprioceptive sensitivity; increased thermal sensitivity; reduced thermal sensitivity; increased pain sensitivity; reduced pain sensitivity; change in vestibular function; change in visuospatial function. |
| Kinetic-Functional Neurocentral Health (H02) | With or without risk of neurocentral kinetic-functional deficiency | Mental functionsII; Movement controlIII; Strength; Structure(segment).IIAlteration of consciousness; cognitive alteration; IIIChange in range of motion; change in motor coordination; change in postural control; change in balance; presence of involuntary movements. |
| Kinetic-Functional Musculoskeletal Health (H03) | With or without risk of musculoskeletal kinetic-functional deficiency | Pain; Joint mobility; Strength; Structure(segment). |
| Kinetic-Functional Respiratory Health (H04) | With or without risk of respiratory kinetic-functional deficiency | OxygenationIV; Respiratory discomfortIV; Lung expansion volumeV; Respiratory muscle strengthVI.IVrest; effort; sleep;V Recruitable component; non-recruitable component;VIInspiratory; expiratory; inspiratory and expiratory. |
| Kinetic-Functional Cardiovascular Health (H05) | With or without risk of cardiovascular kinetic-functional deficiency | Aerobic capacityVII; Functions of vesselsVIII; fatigabilityIX; Heart rateX.VIISlight reduction; moderate reduction; severe reduction; VIIIArterial(mild, moderate, severe); Venous (mild, moderate, severe); lymphatic; IXRest; effort; XWithout medication; with medication. |
| Kinetic-Functional Integumentary Health (H06) | With or without risk of integumentary kinetic-functional deficiency | Sensory functions; Joint mobility; Pain; Structure(segment). |
| Kinetic-Functional Urinary Health (H07) | With or without risk of urinary kinetic-functional deficiency | Bladder functions; Pelvic floor muscle functionXI; Sensations associated with urinary functionsXII; Urinary continenceXIII.XIAlteration of strength; coordination change; relaxation change; resistance change; tonus change; absence of contraction; association of more than one; XIIIncreased feeling of bladder filling; decreased sensation of bladder filling; absence of fullness and desire to urinate; pain and burning urination; sensation of incomplete emptying of urine; XIIIAlteration of effort, alteration of urgency, alteration of effort and urgency; other types of change. |
| Kinetic-Functional Genital Health (H08) | With or without risk of genital kinetic-functional deficiency | Sexual functionsXIV; Pelvic floor muscle functionXI; Pain; Functions associated with menstruation or post-menopauseXV.XIVDesire phase; excitation phase; orgasmic phase; resolution phase; more than one change;XVMenarch; menacme; climacteric; post-menopause/vasomotor alteration. |
| Kinetic-Functional Digestive Health (H09) | With or without risk of digestive kinetic-functional deficiency | Defecation functions – fecal or anal continenceXVI; Pelvic floor muscle function; Pain; Fecal elimination functionsXVII. XVIAlteration of effort, alteration of urgency, alteration of effort and urgency;flatus incontinence; other types of change.XVIIConstipation; diarrhea; change in fecal consistency; change in defecation frequency and fecal consistency; need to use manual or other maneuvers; association of more than one.} |
| Kinetic-Functional Metabolic Health (H10) | With or without risk of metabolic kinetic-functional deficiency | Aerobic capacityVII; Body mass; Body fat; Overall muscle mass. |
| Structure of the Kinetic-Functional Deficiencies chapters (D) | ||
| Organic system | Functional and/or structural status | Variables |
| Neuroperipheral Kinetic-Functional Deficiency (D01) | Eutonic; Hypotonic. | Autonomic function; Strength; Sensory functionsI; Structure(segment).IIncreased tactile and/or proprioceptive sensitivity; reduced tactile and/or proprioceptive sensitivity; increased thermal sensitivity; reduced thermal sensitivity; increased pain sensitivity; reduced pain sensitivity; change in vestibular function; change in visuospatial function. |
| Neurocentral Kinetic-Functional Deficiency (D02) | Eutonic; Hypotonic; Elastic hypertonic; Plastic hypertonic; Floating. | Mental functionsII; Movement controlIII; Strength; Structure(segment).IIAltered level of consciousness; cognitive alteration; IIIChange in range of motion; change in motor coordination; change in postural control; change in balance; presence of involuntary movements. |
| Musculoskeletal Kinetic-Functional Deficiency (D03) | No structural damage; With acute structure injury; With chronic injury structure. | Pain; Joint mobility; Strength; Structure(segment). |
| Respiratory Kinetic-Functional Deficiency (D04) | Obstructive of the upper airways and/or proximal lower airwaysXVII; Obstruction of the middle-distal lower airwaysXVII; Restrictive; Low elastance; Neuromuscular; Not specified.XVIIAirway secretion component; component is not secretion in airways. | OxygenationIV; Respiratory discomfortIV; Lung expansion volumeV; Respiratory muscle strengthVI.IVrest; effort; sleep;V Recruitable component; non-recruitable component;VIInspiratory; expiratory; inspiratory and expiratory. |
| Cardiovascular Kinetic-Functional Deficiency (D05) | No structural change; With structural change. | Aerobic capacityVII; Functions of vesselsVIII; fatigabilityIX; Heart rateX.VIISlight reduction; moderate reduction; severe reduction; VIIIArterial(mild, moderate, severe); Venous (mild, moderate, severe); lymphatic; IXRest; effort; XWithout medication; with medication. |
| Integumentary Kinetic-Functional Deficiency (D06) | No edema; With acute edemaXVIII; With chronic edemaXVIII.XVIIIWithout integrity rupture and without pigmentation alteration; Without rupture of integrity and with alteration of pigmentation; With integrity rupture and without pigmentation alteration; With rupture of integrity and with alteration of pigmentation. | Sensory functions; Joint mobility; Pain; Structure(segment). |
| Urinary Kinetic-Functional Deficiency (D07) | StorageXIX; EmptyingXX; Not specified.XIXWithout urgency; Urgently;XXHesitation; Flow change; Need for effort/urinary retention. | Bladder functions; Pelvic floor muscle functionXI; Sensations associated with urinary functionsXII; Urinary continenceXIII.XIAlteration of strength; coordination change; relaxation change; resistance change; tonus change; absence of contraction; association of more than one;XIIIncreased feeling of bladder filling; decreased sensation of bladder filling; absence of fullness and desire to urinate; pain and burning urination; sensation of incomplete emptying of urine; XIIIAlteration of effort, alteration of urgency, alteration of effort and urgency; other types of change. |
| Genital Kinetic-Functional Deficiency (D08) | No structural change; With structural changeXXI.XXIMild pelvic organ prolapse; Moderate pelvic organ prolapse; Severe pelvic organ prolapse; Complete pelvic organ prolapse | Sexual functionsXIV; Pelvic floor muscle functionXI; Pain; Functions associated with menstruation or post-menopauseXV.XIVDesire phase; excitation phase; orgasmic phase; resolution phase; more than one change;XVMenarch; menacme; climacteric; post-menopause/vasomotor alteration. |
| Digestive Kinetic-Functional Deficiency (D09) | No structural change; With structural change. | Defecation functions – fecal or anal continence; Pelvic floor muscle function; Pain; Fecal elimination functionsXVI.XVIAlteration of effort, alteration of urgency, alteration of effort and urgency;flatus incontinence; other types of change.XVIIConstipation; diarrhea; change in fecal consistency; change in defecation frequency and fecal consistency; need to use manual or other maneuvers; association of more than one. |
| Metabolic Kinetic-Functional Deficiency (D10) | No metabolic dysfunction; With metabolic dysfunction. | Aerobic capacityVII; Body mass; Body fat; Overall muscle mass. |
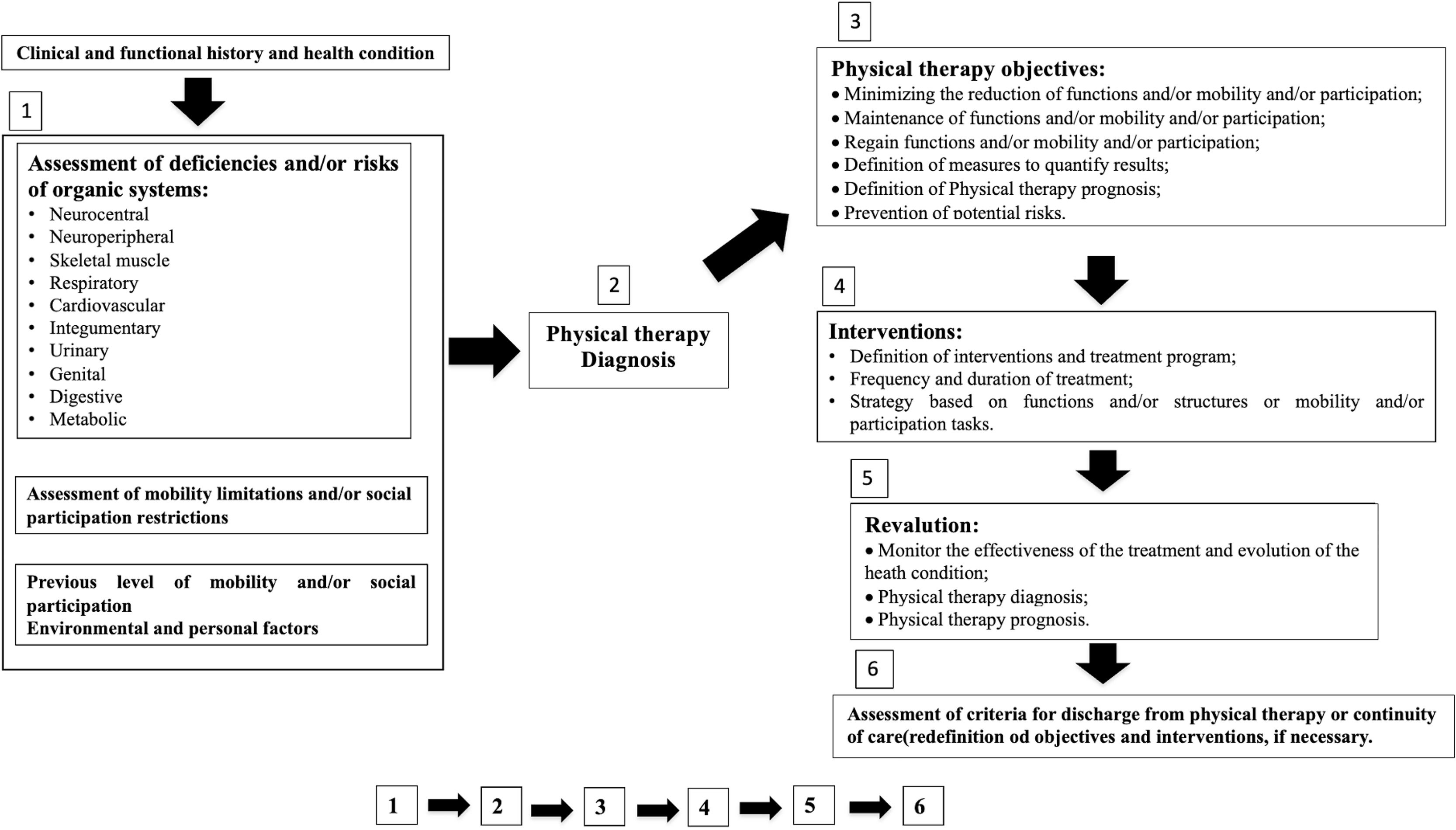
To quantify changes in function and/or structure in the physical therapy diagnosis classification, the use of a 0–4 Likert scale was proposed. In this scale, zero (0) means a change of 0–4% , one (1) indicates a change of 5–24 %, two (2) indicates a change of 25–49 %, three (3) indicates a change of 50–95 % and four (4) indicates a change of 96–100 %. For some variables, the change is rated as dichotomous as zero (0) for no change and four (4) for any amount of change. To identify the risk of physical deficiency, the scale is also dichotomous where zero (0) means no risk and one (1) means a risk of developing physical deficiency. The phases of the physical therapy work process using the diagnosis classification are described in Fig. 2.
DiscussionThe Brazilian Classification of Physical Therapy Diagnosis is a milestone in the history of physical therapy as it fills an existing gap in our profession, by providing an important contribution to defining the physical therapy scope of action, through the description of our outcomes of interest, which are related to our professional specialties and normative documents. This will help the health system, as well as society, to understand the unique role of the physical therapist as a first-contact health professional in primary care, a specialist in human movement working in various specialties with full autonomy to conduct clinical assessment using specific outcome measures. This would allow the prescription of treatment based on a unique physical therapy diagnosis.2–5,10
Another relevant point is that the Brazilian Classification of Physical Therapy Diagnosis has the potential to guide clinical decision-making. The use of this classification tool with validated and reliable diagnostic assessment tools may improve the delivery of care by physical therapists in different healthcare settings.
This diagnostic classification has the potential to expand stakeholder views beyond the biomedical model, increasing the understanding that the individual is much more than a disease or change in health condition. It may expand the care provided based on the ability to perform human movement, from the most basic tasks to those of greater complexity, such as sports, work and leisure.2,5 This is also related to the principle of integrality in health that is part of the Brazilian unified health system, which describes that care must be integral to the individual. Future research related to its validation, reliability, and adherence of the physical therapist to the classification, as well as the identification of the barriers and facilitators for using the classification should be conducted in the future by researchers of different physical therapy specialties.
ConclusionThe Brazilian Classification of Physical Therapy Diagnosis system is an important advance for the physical therapy profession in Brazil, allowing physical therapists to identify structural and/or functional alterations in a simplified and standartised way. This classification may help to consolidate the autonomy of Brazilian physical therapists by establishing a clearer pathway between the diagnosis and interventions.
FundingAll authors declare no specific funding for this contribution.