Patients’ beliefs have an important influence on the clinical management of low back pain and healthcare professionals should be prepared to address these beliefs. There is still a gap in the literature about the influence of patients’ perceptions of their clinical diagnosis on the severity of their pain experience and disability.
ObjectivesTo identify the perceptions of patients with chronic non-specific low back pain regarding the influence of their clinical diagnosis on pain, beliefs, and daily life activities.
MethodsQualitative study of 70 individuals with chronic non-specific low back pain. A semi structured interview was conducted about patients’ beliefs and perceptions regarding the influence of clinical diagnosis on their daily activities and pain intensity.
ResultsMost participants believed that higher number of different clinical diagnoses for the same individual may be associated with high pain intensity and disability for daily activities and that pain and injury are directly related. Patients beliefs were grouped into four main themes: (1) pain has multifactorial explanation in physical dimension; (2) improvement expectation is extremely low in patients with chronic pain; (3) clinical diagnosis influences pain and disability levels; (4) clinical diagnosis is extremely valued by patients.
ConclusionsPatients believe that there is a strong relationship between structural changes in the lower back, pain, and daily life activities; thus, providing evidence of a strong influence of the biomedical model on their beliefs.
The treatment of chronic non-specific low back pain (NSLBP) represents a significant challenge for clinicians and researchers. The multifactorial nature and the lack of association between structural damage and pain are examples of issues that healthcare professionals need to face and manage.1
Patients with NSLBP often present with unhelpful behavioural strategies in an attempt to protect the lumbar region, because many of them believe that functional movements may increase structural damage.2 Patients’ beliefs have an important influence on the clinical management of low back pain, and healthcare professionals should be prepared to address these beliefs.2–8
The holistic biopsychosocial model can be a reasonable approach to manage patients with chronic NSLBP. This model predicts that people can be ill without underlying pathology and it also considers social and behavioral aspects to explain illness and pain. In contrast, the biomedical model is characterized by an approach that attributes illness to a single cause located within the body.9–14
The clinical diagnosis based on the biopsychosocial model usually considers the patient centered care approach and it can manage the multifactorial nature of chronic NSLBP.9 Healthcare professionals with a higher biomedical clinical orientation usually contribute to high levels of fear avoidance beliefs in their patients.10–15
Patients’ beliefs about their health condition, diagnosis, and even treatment options play a fundamental role in clinical management, adherence, and prognosis.5,6,7,10,11
There is still a gap in the literature about the influence of patients’ perceptions of their clinical diagnosis on the severity of their pain experience and daily life activities.Thus, the aim of this study was to identify the perceptions of patients with chronic NSLBP regarding the influence of their clinical diagnosis on pain, beliefs and daily life activities.
MethodsStudy design and ethical considerationsA qualitative study was conducted according to the Standards for Reporting Qualitative Research (SRQR).16 It was previously approved by the ethics committee of the Centro Universitário Augusto Motta (UNISUAM), Rio de Janeiro, RJ, Brazil, under the number 85,716,618.6.0000.5235 and all patients signed an informed consent form.
ParticipantsA convenience sample of 70 patients with chronic NSLBP from three physical therapy outpatient services (in a university hospital, in a private university, and in a public health care unit) in the city of Rio de Janeiro was recruited. Considering the research question and the aims of the study, we also utilized sample saturation as a sampling strategy.17,18 If no new information emerged after five new interviews, stopping data collection was considered. This strategy was applied in all services that patients were interviewed.
Participants over 18 years old with chronic NSLBP were eligible for the study. All eligible participants had to report pain in the area between the 12th rib and buttock crease with or without accompanying non-radicular leg pain as the main pain-related complaint; symptom duration of at least 12 weeks; Oswestry Disability Index score of 14% or more; being able to walk independently (with or without aids); and ability to understand Portuguese well enough to be able to complete the questionnaires. First, the participant received a clinical (structural/pathoanatomical) diagnosis of low back pain by an orthopedist and the possible diagnosis of NSLBP was confirmed by a physical therapist with experience in applying guideline recommended diagnostic triage of low back pain in patients from outpatient services and hospital settings. If the diagnosis of NSLBP was confirmed and the participant met all inclusion criteria, they were included in the study. Patients with known or suspected red flag disorders like fracture, malignancy/cancer, cauda equina syndrome or progressive neurological disorder, inflammatory or infectuous diseases of the spine; rheumatic conditions; suspected or confirmed pregnancy; suspected radicular pain; or spinal or hip surgery < 6 months previously, were excluded from the study. Patients with cognitive inability to complete the questionnaires were also excluded from the study.
Data collection and analysisIn the first step of data collection, we collected sociodemographic and clinical data including age, educational level, and the clinical diagnosis as indicated by the orthopedist. If the individual had more than one clinical (structural/pathoanatomical) diagnosis related to their complaint, previously collected in visits to different orthopedists (e.g. bulging disc, hyperlordosis, arthrosis), all these diagnoses were considered and collected. These data were collected based on self-report in the moment of the interview and to confirm this information, the clinical records of patients were revisited. Diagnoses related to other musculoskeletal and non-musculoskeletal complaints were also identified at the time of the interview based on patients’ self-report. Self-reported psychological disorders (depression, panic disorder, and anxiety) were also collected at the moment of the interview. Participants had to answer Yes or No if they already had any psychological disorders diagnosed by a health professional.
Assessement of pain included pain distribution (i.e. pain body chart) and pain intensity. Pain intensity was measured using the Numerical Pain Rating Scale (NPRS), based on pain at the time of the interview. The NPRS was rated on a scale from 0 to 10 points, with 0 representing ‘no pain’ and 10 ‘the worst possible pain.’ To better characterize the sample, participants also completed the Central Sensitisation Inventory (CSI).19 Disability due to low back pain was measured using the Oswestry Disability Index.20,21 Participants’ characteristics were analysed through descriptive statistics. Shapiro-wilk and Kolmogorov-smirnov Tests were utilized to analyze data distribution. Data were reported as, frequency (proportion) and mean ± standard deviation (SD). Data were analyzed using SPSS version 22 software (SPSS Inc,Chicago, Illinois).
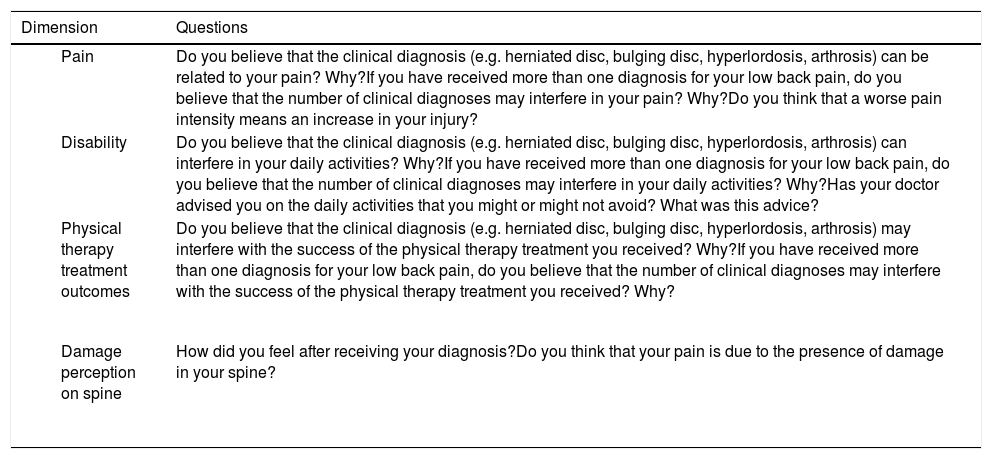
The second step of data collection was the qualitative assessment. A semi-structured interview framework was developed specifically for this study, containing questions related to patients’ perceptions about clinical diagnosis and its influence on their beliefs and daily life activities (Table 1). The interview framework was pilot tested in a physical therapy outpatient service (university hospital) with 7 patients with NSLBP. Subsequently, minor adjustments were made in the semantic of the sentences to improve patient's understanding. We also concluded that a private and quiet room was necessary for the interview. The first author, a physical therapist with experience in outpatient and hospital practice and a PhD student, conducted all the interviews individually. The interviewer received training on how to conduct qualitative research interview and to avoid potential bias. Participants did not know the interviewer and no personal bond was established prior to the interview. The duration of the interview was estimated to last from 15 to 30 min. A smartphone was used to record the conversation.
The semi-structured interview framework.
The qualitative analysis was performed through discourse content analysis.22 The unit of analysis was the fully transcribed audio recording of the interview in the Portuguese language. The translation of the quotes for English language was conducted by two independents translators, with more than 10 years of clinical experience in physical therapy outpatient service, and reviewed by a professional translator. They utilized colloquial language in the quotes as it was presented in Portuguese. The interviews were recorded, transcribed verbatim, and analysed qualitatively using inductive qualitative content analysis. Two of the authors (IB and RA) listened to the recordings and read the transcripts. Both authors are physical therapists, with more than 10 years of clinical experience and had previous theoretical knowledge in qualitative studies. Data were systematically analyzed to determine the meaning units (the similarities and information extracted from discourses). The meaning units were coded and organized into themes and sub-themes, independently by both authors, according to the study objectives.22 The Nvivo 11 software was used for qualitative data management. The definitions of the themes and sub-themes identified in the recordings were discussed by the interviewer and the other author. Where opinions varied, the cases were discussed in an on-line meeting until consensus was achieved. If consensus was not reached, a third author (NM, also a physical therapist with extensive clinical practice experience) was invited to arbitrate. The results were grouped according to the similarities of discourses among individuals, considering the proposed dimensions in the semi-structured interview framework (Table 1).
ResultsParticipants’ characteristicsA total of 70 participants were included. Of these, 49 were undergoing physical therapy treatment during the interview and the remaining participants started the treatment at the same day as the interview. We included 21 participants from the university hospital outpatient service, 23 from the private clinic and 26 from the public health care unit. All participants were recruited from the musculoskeletal rehabilitation units of all services.
The data were normally distributed. The mean ± SD age of the participants was 60.7 ± 13.7 years, the majority of the sample was female (83%) and had a mean of 9.3 ± 4.6 years of formal education. Regarding clinical characteristics, the mean score on the CSI was 50.8 ± 12.2 points and on the Oswestry Disability Index was 31.7 ± 14.8 points, mean pain intensity was 6.3 ± 2.6 points and pain duration was 116.6 ± 127.8 months. The most common clinical (structural / pathoanatomical) diagnosis related to the patients’ low back pain was lumbar spondylosis followed by intervertebral disc injuries (e.g. dehydration, bulging disc, disc protrusion). There was also a high prevalence of self-reported psychological disorders (depression, panic disorder, and anxiety). A total of 13 patients received one diagnosis, 26 received two diagnoses, and 31 had received three or more diagnoses since their first episode of low back pain. A total of 44 patients had received some advice from a health professional. Among these patients, 41 received movement avoidance advice.
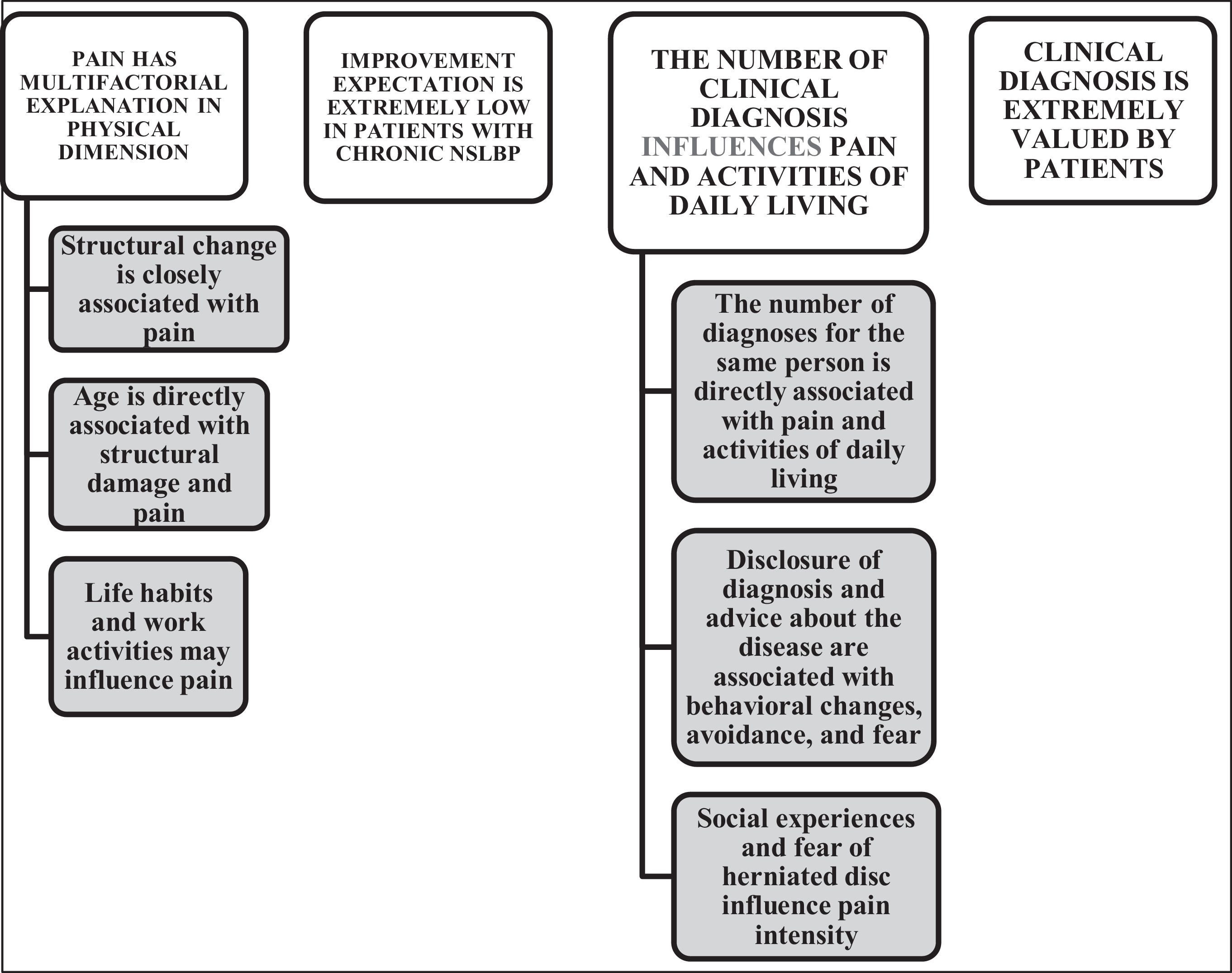
Qualitative resultsThe analysis of the recordings’ content identified similarities and the perceptions of participants were grouped into themes and sub-themes (Fig. 1). The results indicated four themes: (1) pain has a multifactorial explanation in physical dimension; (2) improvement expectation is extremely low for chronic NSLBP; (3) the number of clinical diagnosis influences pain and activities of daily living; (4) clinical diagnosis is extremely valued by patients. We did not find relevant differences in patient`s discourses between the three different clinical settings where data were collected.
Pain has a multifactorial explanation in the physical dimensionParticipants reported several possible factors for explaining low back pain. All variables reported by the patients present a close relation to structural damage. Participants considered only the physical dimension of pain as an explanation for their chronic NSLBP.
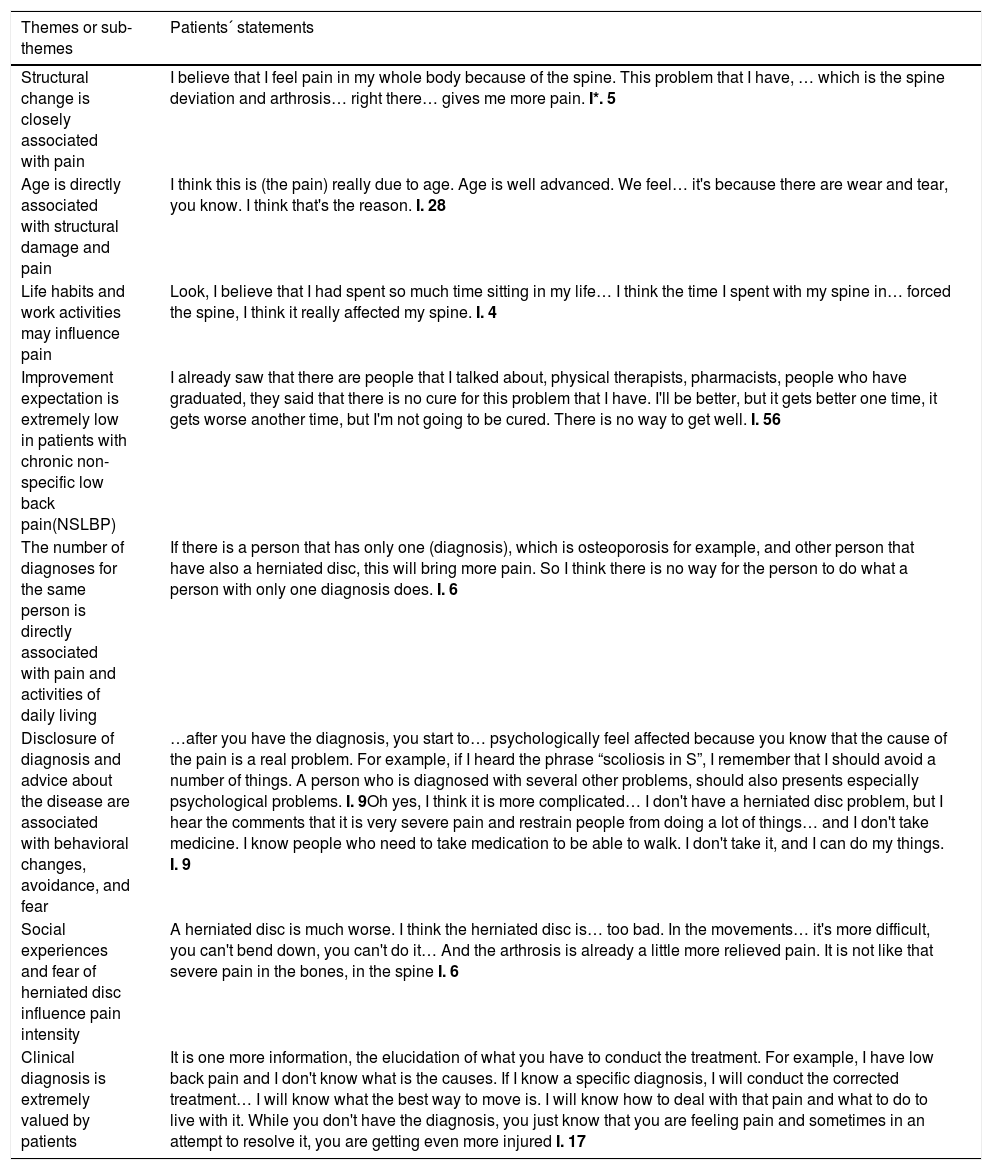
Structural change is closely associated with pain Participants often interpreted that their pain was associated with the presence of vertebral degeneration found in the spine. In addition, participants also believed that pain intensity was dependent on the number of imaging findings as well as the duration of symptoms.
If you feel much pain, you have to look for treatment because your injury is already advanced. I think the more pain you feel, the more advanced is the tension in your muscles. These little cushions that have been wearing away, some come with a parrot beak that causes the so famous disc herniation [Interview (I.) 54].
Table 2 presents other statements that support the themes identified after patients’ discourse analysis.
Patients` statements that supports the themes and sub-themes found in the qualitative analysis.
Legend: * I. Identification of the Interview number.
Participants reported that over the years the lumbar region might suffer structural damage due to the ageing process. This might be a result of ‘inadequate’ movements that they performed throughout their lives.
So, I also think it depends on the age of the person. Because I started to have problems with older age. Because of menopause, bone mass loss begins, some muscles and nerves start to get overloaded, the cells are dying, so I think many people may feel that way because of their age. Age influences a lot. I'm feeling it. Because before I did these activities and my spine had no problem, but because of my age, after 40, I started to see the difference … Then after I started in the climacteric phase it is getting worse (I. 57).
Life habits and work activities may influence painParticipants believe that life style contributes to spinal overload and consequently pain. They also believe that prolonged static posture during work activities and excessive repetitive movements required in work activities are associated with chronic NSLBP. Is also due to my work. I have to work sitting down for a long while and I think that it can influences a lot. … If I could lost some weight, I believe that it could also help (I. 64)
Improvement expectation is extremely low in patients with chronic NSLBPParticipants believe that some improvement can be achieved by treatment, but that there are no clinical approaches or technological tools that can fully restore their health.
I already knew that I had a back problem, so I got discouraged from there (medical appointment). He said that my spine was impaired.” Then he said: “Oh, I don't know what to do with you. Oh, scoliosis is beginning, your spine is so worn out.” I said: “Doctor, what am I going to do now? I need my spine.” He said: “Look, let's treat, but there is no cure” (I. 40).
The number of clinical diagnosis influences pain and activities of daily livingParticipants believe that people with various diagnoses are more likely to have higher levels of pain and more difficulties in activities of daily living. Participants report that having multiple diagnoses means that the lumbar spine is severely injured.
So, I think the more situations (diagnoses) you have, the more pain you will have… If it's just one thing (diagnoses), it's a type of pain, if it's three, I believe the level of pain is much greater (I. 4).
I started (on the beginning of my problem) with one diagnosis and now I have four different problems associated with my spine. Nowadays I am worst, I can`t do everything that I wish because I have pain (I. 35) Disclosure of diagnosis and advice about the disease are associated with behavioural changes, avoidance, and fear
Participants reported how their lives changed after receiving their clinical diagnoses and treatment recommendations to manage their low back pain. The way the health professional communicates their clinical diagnosis seem to shape patient beliefs. Incorrect information provided by health professionals, such as poor prognosis for patients with chronic NSLBP, influenced participants to view their diagnosis as threatening and as the reason for changing their daily activities:
I was sad. Although I was 68 years old, I liked to play soccer, I still like it and to do exercise, but he forbade me. I was upset. I was sad because it limited me. I started worrying, trying to correct the posture. I've already avoided many things which I like to do. But unfortunately, it has to be treated (I. 43).
Social experiences and fear of herniated disc influence pain intensityParticipants reveal how their beliefs about diagnosis, pain, and disability were influenced by other people's experiences. The social context also seems to influence beliefs about the clinical diagnosis of chronic NSLBP. The most threatening diagnosis mentioned was herniated disc and it appeared in different moments of the patients’ discourse. Although no patient included in the study had signs and symptoms of radiculopathy, the diagnosis of disc herniation seems to be the most feared by patients:
The person who has this herniated disc problem should feel more pain. More pain to do any activity… Because I think it's a more serious problem in the spine. It is harder for the person to move, to sit, to lift a load. … and when I go to the doctor, we talk, and we listen to things. It can help or not. But I try to listen to other problems to compare with mine. (I. 5).
Clinical diagnosis is extremely valued by patientsPatients often expect to receive a diagnosis and an explanation for the cause of their pain. Participants believe that a clinical diagnosis is critical to the successful treatment of their painful condition. The absence of a clinical diagnosis generates a feeling of apprehension and fear about not knowing what is going ‘wrong’ in the low back.
When I received the diagnosis, I could have started a correct treatment and to avoid some movements that could bring me more pain. When you don`t have a disgnosis, you don`t have a real explanation for your symptoms… and you can do some movements that bring problems to your spine. (I.17).
DiscussionOur findings indicate that clinical diagnosis can influences the perception about pain, treatment beliefs, and daily life activities of patients with chronic NSLBP. The themes identified in this study suggest that there is a perception of a strong relationship between structural changes (i.e. findings on imaging exams), pain, and daily life activities, suggesting that patients rely on the biomedical model to explain their condition.
To the best of our knowledge, the present study is the first to utilize a qualitative perspective to report patients’ beliefs and their influence about pain intensity, daily life activities, and the relationship with the clinical diagnosis(es) they received. Nevertheless, other findings reported in the literature are consistent with our results.23–27 The study by Jenkins et al.27 showed that patients believed that an imaging exam should be performed before receiving a specific treatment for low back pain.27 Curiously, there is evidence that imaging can generate a negative effect in patients with low back pain27 leading to higher pain intensity and lower overall health perception compared to patients who have not undergone imaging.29–31
The present study also identified how patients view the influence of their diagnosis on their pain and daily life activities and also found that it can impact patient's expectations about their prognosis. One important example that we found in a patient discourse can illustrate this belief “My pain may last forever, because lumbar spondylosis has no cure (Interviewed 39)”. This kind of diagnosis can be threatening for patients and healt care professionals should know how to deal with this patient perception. The study by Hsu et al.32 also found similar results.
Considering our findings, clinicians should be aware of the impact of how they communicate to patients to minimize any negative effects.4,14,33,34 Clinicians should be trained on how to address the biopsychosocial aspects of pain and to improve their verbal and non-verbal communication skills to be able to deliver more appropriate care34,35 and treatments that address the multidimensional aspects of pain.36–41
The present study also identified that patients with chronic NSLBP need information about their condition, and more specifically, an explanation of their symptoms. However, the clinical diagnosis based on musculoskeletal structure and solely on physical factors is often seen as just a label which usually is not enough to explain pain and disability in this population. Patients should also understand that social and behavioral components can be involved in chronic NSLBP and health professionals must be able to offer patient-centered care.37,39,42
Paradoxically, some participants reported relief and comfort immediately after receiving their clinical diagnosis. These attitudes seem to be based on the belief that a clinical diagnosis is essential for treatment, and also on the thought that their pain is due to a severe pathology. In contrast with these patients' beliefs, there is a considerable body of evidence to suggest that structural diagnosis or findings commonly found in imaging exams are not enough to explain the cause of pain in this popuplation.28,30,31,38,39,42,43
The influence of clinical diagnosis on the beliefs of patients with chronic NSLBP is lacking in the literature. Therefore, we aimed to fill this gap, highlighting the need for better understanding of how clinical diagnosis can impact patients with chronic NSLBP. The findings of the present study draw attention to the need for a thorough reflection on the impact of the initial approach and discourse of the health professional throughout the treatment course, which can generate a nocebo effect and influence the beliefs of patients.
LimitationConsidering the scope and design of the study, as we studied patients’ beliefs, caution is needed to assume that clinical diagnosis can influence pain intensity and the performance of daily life activities in patients with chronic NSLBP. The semantic structure of the questions inserted in the interview is another point that we should consider. Some of them were directive and dichotomous to facilitate comprehension. Even using a reflexive question on the end of the sentences, the patients could be biased or some information could not be captured.
ConclusionThe present study identified how patients view the influence of their diagnosis on their pain and daily life activities. In addition, patients’ beliefs indicate that they attributed multiple physical causes for pain, but didn`t consider the multifactorial nature of chronic NSLBP. Patients had low expectations of improvement and valued receiving a clinical diagnosis. Importantly, patients believe that pain intensity was dependent on the number of imaging findings as well as the duration of symptoms. There is a strong relation between findings in scans in the lower back, pain, and daily life activities; evidencing a strong influence of the biomedical model on their beliefs.
This study was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Brazil) and Fundação Carlos Chagas Filho de Amaro à Pesquisa do Estado do Rio de Janeiro (FAPERJ, Rio de Janeiro).