After cardiac surgery, physiological abnormalities or adverse events might occur in patients in the intensive care unit (ICU) during physical therapy care. Identifying these events may help improve patient safety and care.
ObjectivesTo estimate the incidence and the degree of severity of physiological abnormalities or adverse events during physical therapy interventions provided in the ICU after cardiac surgery. To explore the relationship between these events and patients’ characteristics and clinical outcomes.
MethodsProspective observational study of adult patients in the postoperative period of cardiac surgery admitted to the ICU of a referenced university hospital. Physical therapy interventions were observed by a team trained to evaluate and register the occurrence of physiological abnormalities or adverse events and grading their consequences. We compared baseline characteristics and outcomes of patients with versus without these events.
ResultsWe observed 935 physical therapy interventions in 323 patients, of which 189 (20%, 95% confidence interval: 18, 23%) resulted in physiological abnormalities or adverse events. The highest incidences of these events were observed during endotracheal suctioning (44%), walking (40%), and noninvasive ventilation (37%). Hemodynamic changes were the most frequent events accounting for 74% of all events. Only 2% of interventions resulted in mild harm and 0.2% in moderate harm. The presence of comorbidities was associated (p = 0.03) with the occurrence of these events.
ConclusionPhysiological abnormalities or adverse events occurred in 20% of physical therapy interventions in patients in the ICU after cardiac surgery, with 10% of those resulting in negative effects. Only the presence of comorbidities was associated with the occurrence of these events.
Physical therapy is a non-pharmacological treatment approach that plays an essential role in the care of patients undergoing cardiac surgery. Studies have reported that physical therapy is important to prevent or minimize complications in the postoperative period and may improve patients’ clinical outcomes.1–5 Postoperative physical therapy interventions vary across hospitals and countries but can include discontinuation of invasive mechanical ventilation (MV), airway clearance, maintenance of spontaneous ventilation, lung expansion, cough stimulation, positioning, and early mobilization.1,6–8
Safety monitoring in most clinical trials of physical therapy interventions have reported minimal or no adverse events.9–11 However, interventions in clinical trials are usually performed in specific populations by highly trained physical therapists, and with very strict criteria for interrupting sessions. Observational studies evaluating the safety of physical therapy in routine clinical care found that physiological abnormalities or adverse events (any untoward medical occurrence in a patient, for example oxygen desaturation and arrythmia) are more likely than expected to occur in critically ill patients in the intensive care unit (ICU).12,13
Safe postoperative care is one of the cornerstones of successful management of patients undergoing cardiac surgery. Because this population is physiologically unstable and might become critically ill, the occurrence and impact of adverse events and the identification of preventable adverse events may help the development of strategies to improve quality of healthcare and patient safety.14–20
We hypothesized that patients after cardiac surgery would have physiological abnormalities or adverse events during ICU physical therapy care and that these physiological abnormalities or adverse events would be associated with poor clinical outcomes. Therefore, we designed a prospective observational study to estimate the incidence of physiological abnormalities or adverse events during ICU physical therapy care in patients after cardiac surgery. The secondary objectives included: 1) to measure the degree of severity of adverse events; and 2) to explore the relationship between the occurrence of adverse events with patients’ baseline characteristics and clinical outcomes.
MethodsStudy design and ethicsThis was a prospective observational study performed at Instituto do Coração (InCor), Hospital das Clínicas, School of Medicine, Universidade de São Paulo (HCFMUSP), Brazil, from June 2016 through November 2017. The study protocol was approved by the Ethics Committee of InCor-HCFMUSP (reference number 1.391.854), and informed consent was waived due to the observational nature of the study. The protocol is registered at ClinicalTrials.gov (NCT03552887).
PatientsWe included patients who underwent elective cardiac surgery and were admitted to the ICU, aged ≥18 years old, and who received at least one physical therapy intervention during ICU stay. Exclusion criteria were medical diagnosis of cognitive or neurological impairments. We screened patients for inclusion in the study two days per week, during the study period, according to a schedule previously determined by the main investigator and the availability of the researchers. Eligible patients were recruited through consecutive sampling method.
Data collectionThe electronic medical record system was used to obtain the patients’ baseline characteristics (i.e., age, sex, body mass index, comorbidities, type of surgery, history of cardiac surgery) and to calculate the European System for Cardiac Operative Risk Evaluation (EuroSCORE) score. The EuroSCORE is a risk stratification tool for postoperative mortality of cardiothoracic surgery and is available at www.euroscore.org.21 One researcher was in charge of tracking the adverse events that occurred during each physical therapy intervention. The physical therapist who provided care to the patient was an ICU staff not involved in the study.
Patients were assessed throughout the period they stayed in the ICU and received physical therapy. The primary outcomes were the occurrence of physiological abnormalities or adverse events and the severity of such events. We recorded the events that happened while receiving physical therapy care in the ICU, and we followed patients until hospital discharge to register the hospital length of stay, mortality, and survival at 28-day/discharge. We also collected information on the need of cardiopulmonary bypass and tracheostomy, duration of cardiopulmonary bypass, and mechanical ventilation. We collected and managed all study data using Research Electronic Data Capture (REDCap).22
Physical therapy interventionsPhysical therapy interventions administered to patients undergoing invasive MV consisted of manual hyperinflation, endotracheal suctioning, and passive mobilization. Mobilization in extubated patients included active exercises, sitting on the edge of the bed, transferring from bed to chair, standing and walking; and respiratory interventions included breathing exercises, airway clearance techniques, lung expansion techniques, intermittent positive pressure breathing (IPPB), noninvasive ventilation (NIV), and nasotracheal suctioning.
All interventions were performed following the standard of care based on strict local clinical guidelines. Each type of intervention was evaluated only once for each patient included in the study. We observed all physical therapy sessions that each intervention was performed for the first time to each patient.
Physiological abnormalities or adverse eventsWe defined 12 types of physiological abnormalities or adverse events, adapted from the study by Zeppos et al.12: 1) changes in mean arterial pressure, less than or greater than 20% of baseline value; 2) heart rate change, less than or greater than 20% of baseline; 3) pulmonary artery pressure change, less than or greater than 20% of the baseline value; 4) arrhythmia; 5) peripheral desaturation of oxyhemoglobin, values lower than 4% of baseline; 6) alteration in level of consciousness; 7) dizziness or vertigo; 8) accidental removal of catheters or tubes; 9) accidental extubation, when there is withdrawal of the endotracheal tube not programmed by the ICU team; 10) fall, unintentional movement of the body to a level lower than the initial position; 11) loss of muscle tone without fall; 12) pneumothorax.
Severity of physiological abnormalities or adverse eventsPhysiological abnormalities or adverse events were classified according to the symptomatic consequence to the patient, using a severity scale ranging from I to V, based on InCor - HFMUSP Patient Safety Subcommittee criteria, literature review, and expert opinions. Grade I (near miss), when the potential incident did not affect the patient, by being detected before it happened (e.g. an increase heart rate greater than 20% during Physical Therapy interventions that returned to baseline without vasoactive drug doses adjustment); grade II (mild harm), when mild symptoms and/or loss of function occur, and/or there is minimal or intermediate harm of short duration with minimal intervention required; grade III (moderate harm), requires significant intervention of the team and/or needs increase of stay, and/or causes long-term harm or loss of function; grade IV (severe harm), life-threatening consequences and urgent intervention indicated; and grade V (death), death caused or anticipated by the adverse event (Supplemental online material).
Statistical analysisContinuous variables with normal distribution are presented as mean ± standard deviation, continuous variables of non-normal distribution are presented as median [interquartile range], and categorical variables as frequency (proportion). For evaluation of normality, we used the Shapiro-Wilk Test. The statistical analysis was performed using the software R Programming (R Core Team, Vienna, Austria; URL: https://www.R-project.org) and was considered statistically significant if the p value was less than 0.05.
The primary outcome variables were the incidence of physiological abnormalities or adverse events (continuous) and the consequences of such events. For inferential analysis, the 95% confidence interval (CI) for proportion was calculated. Based on the maximal incidence's tertiles of adverse events observed in previous studies,18 we categorized the incidence as low <20%), moderate (20–40%), and high (>40%). Our calculated sample size was 323 patients, based on a rate of adverse events in ICU patients of 30%, considering a margin of error of 5%, to obtain estimates with 95% CI.
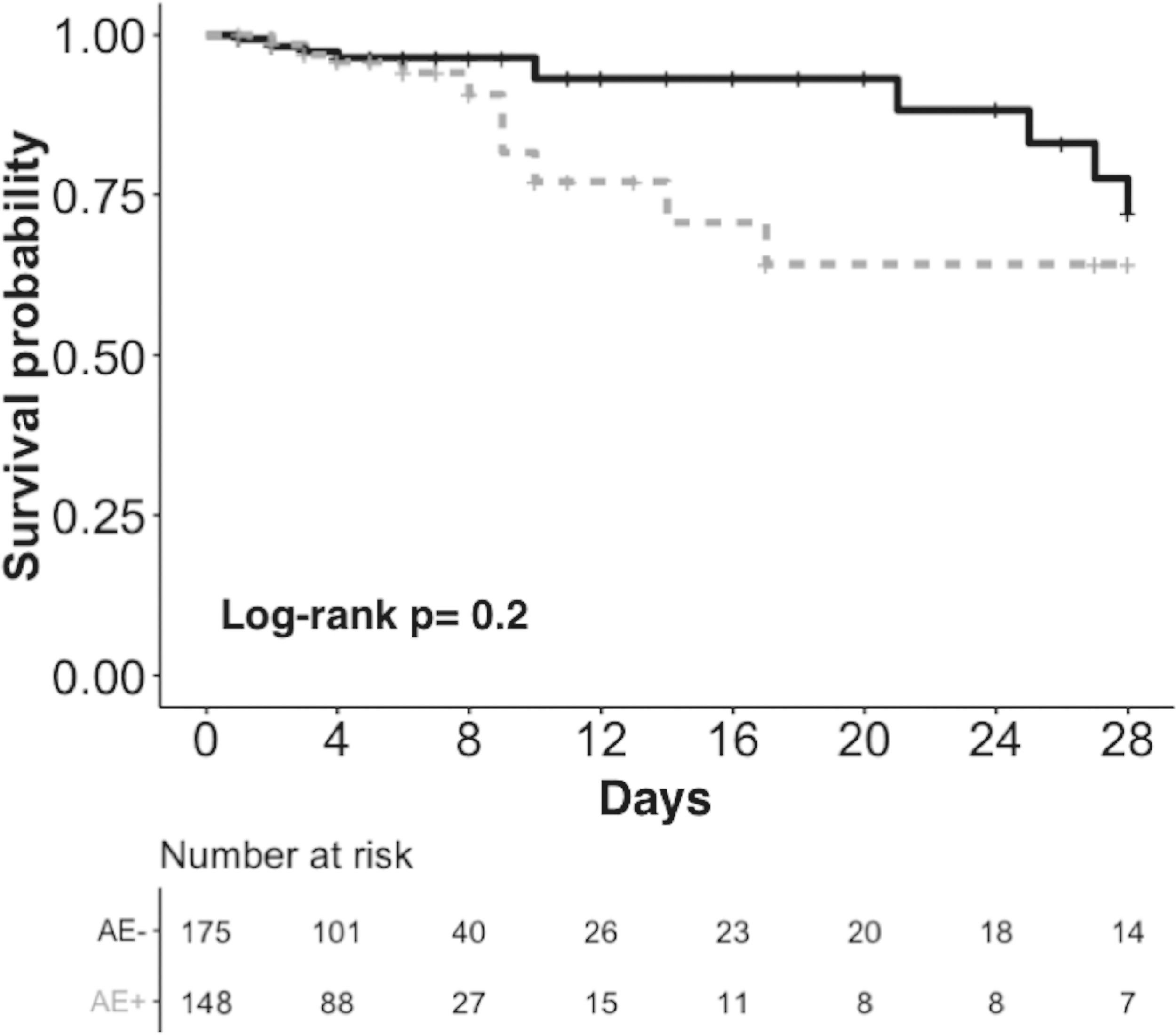
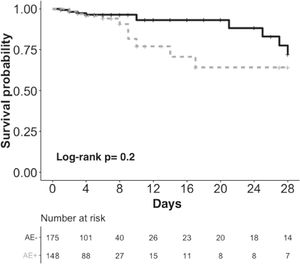
For secondary analysis, qualitative data were compared using χ2 test or Fisher test, and quantitative data were compared using Mann-Whitney test or t-test. To assess the relationship between survival and the incidence of physiological abnormalities or adverse events, we constructed Kaplan-Meier curves, right censoring patients who were discharge home before 28 days, and comparison was based on log-rank test.
ResultsDuring the study period, 1841 patients were admitted to the surgical ICU, and 323 patients were included in the study, in which 935 physical therapy interventions were observed. Forty-six percent of patients had at least one physiological abnormality or adverse event during physical therapy interventions (Supplemental online material).
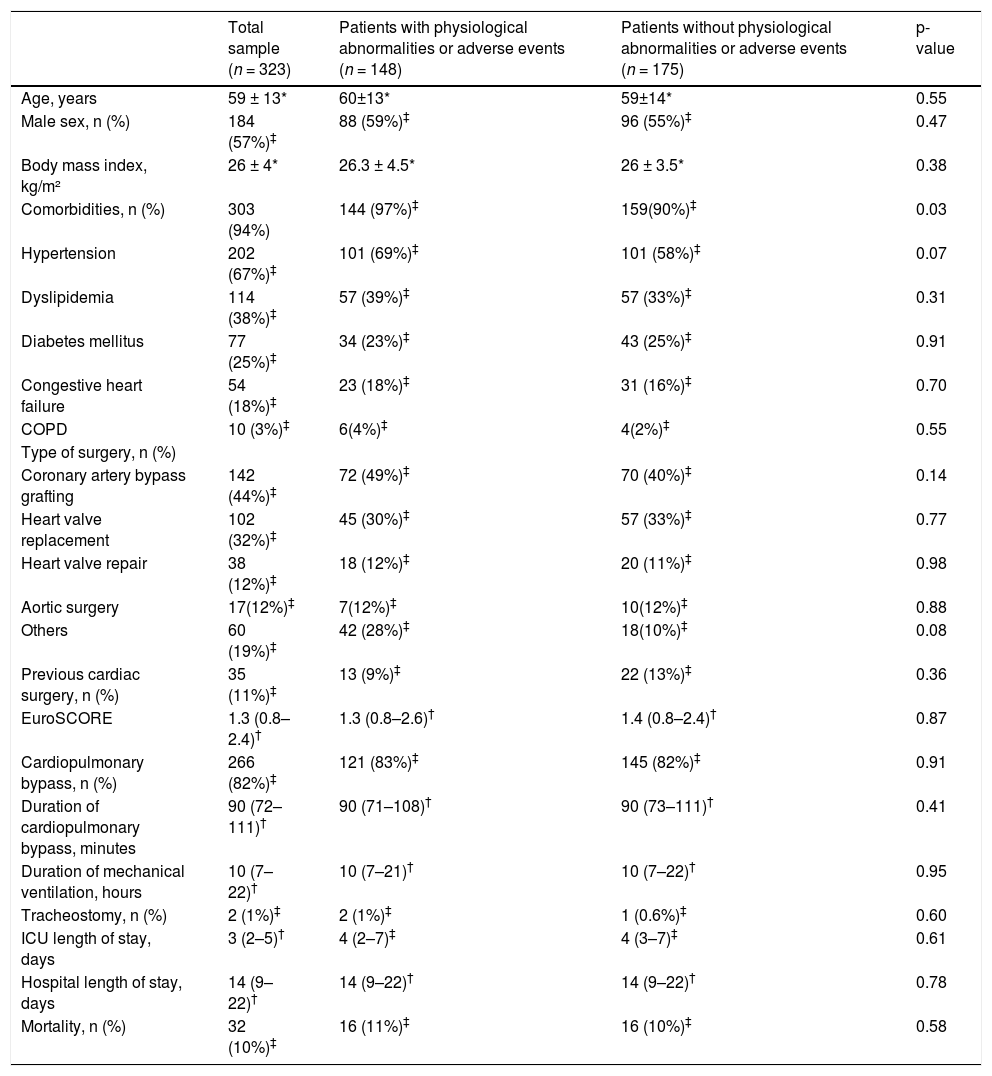
Patient's baseline characteristics and outcomes are summarized in Table 1. The mean age was 59±13 years old, 184 (57%) participants were males, and mean body mass index was 26±4 kg/m². The most frequent surgical diagnoses were myocardial revascularization, valve replacement, and valve repair, with 266 (82%) patients requiring cardiopulmonary bypass. Median EuroSCORE was 1.3 (0.8–2.4), indicating a low early mortality risk group,21 and overall mortality of 10% (32 deaths). The median duration of MV was 10 (7–22) hours, and ICU and hospital length of stay were 3 (2–5) days and 14 (9–22) days.
Patient's baseline characteristics and outcomes in the total sample and according to the incidence of physiological abnormalities or adverse events.
| Total sample (n = 323) | Patients with physiological abnormalities or adverse events (n = 148) | Patients without physiological abnormalities or adverse events (n = 175) | p-value | |
|---|---|---|---|---|
| Age, years | 59 ± 13* | 60±13* | 59±14* | 0.55 |
| Male sex, n (%) | 184 (57%)‡ | 88 (59%)‡ | 96 (55%)‡ | 0.47 |
| Body mass index, kg/m² | 26 ± 4* | 26.3 ± 4.5* | 26 ± 3.5* | 0.38 |
| Comorbidities, n (%) | 303 (94%) | 144 (97%)‡ | 159(90%)‡ | 0.03 |
| Hypertension | 202 (67%)‡ | 101 (69%)‡ | 101 (58%)‡ | 0.07 |
| Dyslipidemia | 114 (38%)‡ | 57 (39%)‡ | 57 (33%)‡ | 0.31 |
| Diabetes mellitus | 77 (25%)‡ | 34 (23%)‡ | 43 (25%)‡ | 0.91 |
| Congestive heart failure | 54 (18%)‡ | 23 (18%)‡ | 31 (16%)‡ | 0.70 |
| COPD | 10 (3%)‡ | 6(4%)‡ | 4(2%)‡ | 0.55 |
| Type of surgery, n (%) | ||||
| Coronary artery bypass grafting | 142 (44%)‡ | 72 (49%)‡ | 70 (40%)‡ | 0.14 |
| Heart valve replacement | 102 (32%)‡ | 45 (30%)‡ | 57 (33%)‡ | 0.77 |
| Heart valve repair | 38 (12%)‡ | 18 (12%)‡ | 20 (11%)‡ | 0.98 |
| Aortic surgery | 17(12%)‡ | 7(12%)‡ | 10(12%)‡ | 0.88 |
| Others | 60 (19%)‡ | 42 (28%)‡ | 18(10%)‡ | 0.08 |
| Previous cardiac surgery, n (%) | 35 (11%)‡ | 13 (9%)‡ | 22 (13%)‡ | 0.36 |
| EuroSCORE | 1.3 (0.8–2.4)† | 1.3 (0.8–2.6)† | 1.4 (0.8–2.4)† | 0.87 |
| Cardiopulmonary bypass, n (%) | 266 (82%)‡ | 121 (83%)‡ | 145 (82%)‡ | 0.91 |
| Duration of cardiopulmonary bypass, minutes | 90 (72–111)† | 90 (71–108)† | 90 (73–111)† | 0.41 |
| Duration of mechanical ventilation, hours | 10 (7–22)† | 10 (7–21)† | 10 (7–22)† | 0.95 |
| Tracheostomy, n (%) | 2 (1%)‡ | 2 (1%)‡ | 1 (0.6%)‡ | 0.60 |
| ICU length of stay, days | 3 (2–5)† | 4 (2–7)‡ | 4 (3–7)‡ | 0.61 |
| Hospital length of stay, days | 14 (9–22)† | 14 (9–22)† | 14 (9–22)† | 0.78 |
| Mortality, n (%) | 32 (10%)‡ | 16 (11%)‡ | 16 (10%)‡ | 0.58 |
EuroSCORE, European System for Cardiac Operative Risk Evaluation; ICU, intensive care unit.
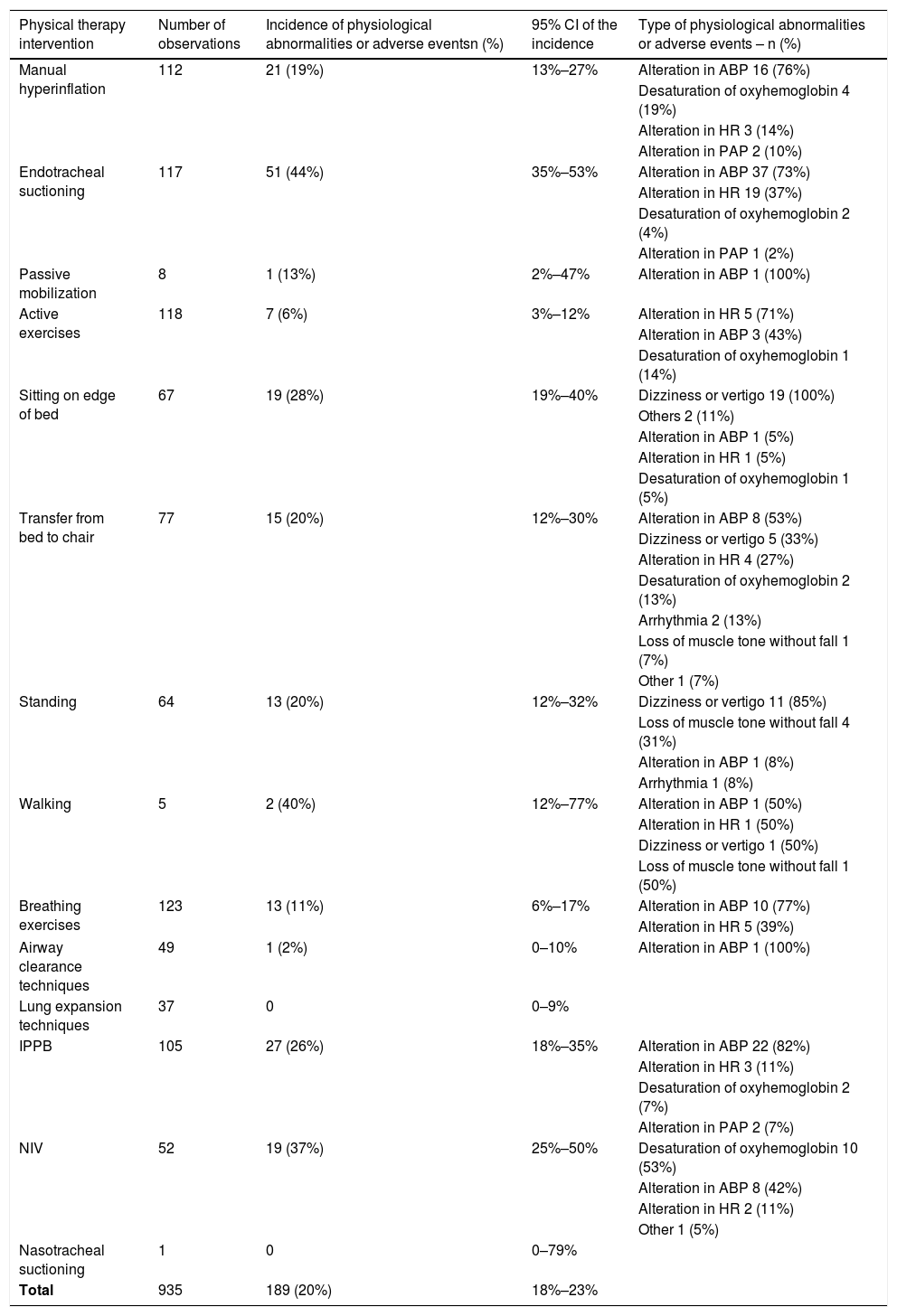
Physiological abnormalities or adverse events had higher incidence during physical therapy interventions in patients undergoing invasive MV (31%, 95% CI: 25, 37%), than during mobilization (17%, 95% CI: 13, 21%) and respiratory interventions (16%, 95% CI: 13, 21%) in extubated patients.
Physiological abnormalities or adverse events that occurred during the physical therapy interventions are described in Table 2. The total incidence of these events among the 935 physical therapy interventions was 20% (95% CI: 18, 23%). The intervention that had the highest incidence of physiological abnormalities or adverse events in patients undergoing invasive MV was endotracheal suctioning (44%, 95% CI: 35, 53%). In extubated patients the highest incidences for mobilization interventions were observed during walking (40%, 95% CI: 12, 77%) and sitting on the edge of the bed (28%, 95% CI: 19, 40%), and noninvasive ventilation (NIV) (37%, 95% CI: 25, 50%) and IPPB (26%, 95%CI: 18, 35%) for respiratory interventions. Only 32 (9.9%) patients had more than one event.
Incidence of physiological abnormalities or adverse events during physical therapy interventions.
CI, confidence interval; ABP, arterial blood pressure; HR, heart rate; PAP, pulmonary arterial pressure; IPPB, intermittent positive pressure breathing; NIV, noninvasive ventilation.
Hemodynamic changes represented 74% of all physiological abnormalities or adverse events. Hemodynamic changes were more frequent in patients receiving invasive mechanical ventilation and during the respiratory interventions in the extubated patients. During mobilization in extubated patients, dizziness or vertigo were more common (Table 2).
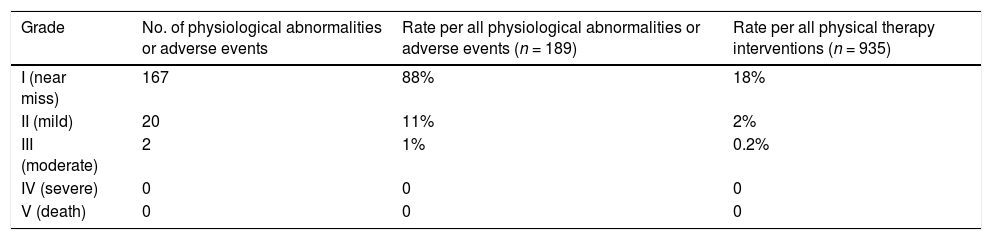
Table 3 shows the incidence of physiological abnormalities or adverse events according to the degree of severity. There was a higher incidence of grade I (near miss), and between all the interventions observed, only 2.2% resulted in adverse events evolving with some harm (grades II and III). No patient evolved with severe harm or death (grades IV and V, respectively).
Comparing patients with or without physiological abnormalities or adverse events, only the presence of comorbidities was associated with occurrence of those events. There was no difference between median duration of MV, median length of ICU and hospital stay, and mortality rate (Table 1). In our sample, the Kaplan-Meier method estimated that the 28-day survival rates for patients without and with physiological abnormalities or adverse events were 72% (95%CI: 55, 94%) and 64% (95%CI: 46, 89%), respectively. However, the log-rank test, used to compare survival curves from patients with versus without events, did not show a statistically significant difference (Figure 1).
Survival analysis at 28 days after cardiac surgery according to occurrence of physiological abnormalities or adverse events. Footnote: The gray dashed line represents patients with physiological abnormalities or adverse events (AE+), and the black line represents patients without physiological abnormalities or adverse events (AE-).
In this prospective observational study of 935 physical therapy interventions in 323 adult patients in ICU, physiological abnormalities or adverse events occurred in approximately 50% of patients who underwent cardiac surgery. The major findings of our study were: (1) physiological abnormalities or adverse events during physical therapy interventions were frequent, especially in mechanically ventilated patients; (2) these events were more common during endotracheal suctioning, walking, and NIV; (3) the most common types of events in mechanically ventilated patients and during respiratory interventions in extubated patients were hemodynamic changes, whereas dizziness or vertigo were more common during mobilization in extubated patients; (3) less than 3% of physical therapy interventions resulted in adverse events evolving with some harm; (4) the presence of comorbidities was associated with physiological abnormalities or adverse events; and (5) the occurrence of these events was not associated with worse clinical outcomes (e.g. longer ICU length of stay or increased mortality).
To our knowledge, this is the first study to focus on reporting the incidence of physiological abnormalities or adverse events in cardiac surgery patients in the ICU through direct observation of physical therapy sessions. Previous studies have focused on ICU team reports,12,13 i.e., events reported in the patient's medical record. We believe that this is a better strategy to assess the safety of physical therapy interventions, because when health care professionals classified events as incidents, critical incidents, or near misses, there are many factors that can influence their decision about whether to file incidence reports, such as the severity of the scenario's impact, its classification, and the practitioner's perceived role in reporting the incident, and they may not always report them or report with substantially curtailed gaps.23,24
In our study, the incidence of physiological abnormalities or adverse events among physical therapy interventions in the ICU was higher than that reported in previous similar studies. Zeppos et al.12 also assessed the occurrence of physiological changes or adverse events over a three-month period in five ICUs and found an incidence of 0.2% between all interventions. We believe that possible explanations are the different types of data collection, and the characteristics of study population.
Sricharoenchai et al.13 monitored 5267 physical therapy sessions conducted in 1110 patients in the ICU, and they found that a total of 34 (0.6%) sessions had a physiological abnormality or potential safety event. This lower incidence may be due to the definitions of adverse events used, which had higher cutoffs, e.g. mean arterial blood pressure above 140 mm Hg or below 55 mm Hg.
We found that physiological abnormalities or adverse events are more common in patients undergoing invasive mechanical ventilation, especially during endotracheal suctioning. During that intervention, hemodynamic abnormalities were the most frequent. However, as we observed only the first time each intervention was performed, all respiratory interventions in patients under MV were observed in the immediate postoperative period. So, we cannot exclude that these events occurred because of a more critical condition.
Maggiore et al.25 analyzed the incidence of adverse events related to endotracheal suctioning. They found a lower rate of 12.4%, compared to our detected rate (44% of observed endotracheal suctioning), which can be explained by the fact that in our study alterations with values beyond those considered in their study were classified as adverse events.
Physiological abnormalities or adverse events were also common in mobilization during sitting on the edge of the bed, transfer from bed to chair, standing, and walking. Hemodynamic changes tend to occur mainly in patients whose bedtime is too long.13 Previous studies have reported that bedside sedation exercises are the most likely to result in changes in heart rate and blood pressure, because position transition generates a potential for cardiovascular changes, and may limit the activity during the physical therapy session, especially in cardiac surgery patients.13,26
Other adverse events highlighted in our study were dizziness, vertigo, and loss of muscle tone without falling. These findings are similar to those reported by previous studies.7,26 A recent analysis26 of the safety of early mobilization after cardiac surgery in 53 patients suggested that this is a safe procedure in the ICU, even if it could be associated with significant hemodynamic alterations. Due to cardiovascular system impairment after cardiac surgery, they recommended that mobilization in the early postoperative period should be performed under strict clinical and hemodynamic monitoring, with particular attention to blood lactate and central venous saturation.
In respiratory physical therapy in extubated patients, physiological abnormalities or adverse events were more common during NIV, especially hemodynamic changes. NIV has been presented as an efficient intervention in patients undergoing cardiac surgery, by improving vital capacity and gas exchange, reducing work of breathing and preventing postextubation acute respiratory failure.27–29 On the other hand, the application of intrathoracic positive pressure, as previously mentioned30 and observed in our study, can produce significant hemodynamic changes.
We believe that physical therapy interventions after cardiac surgery in the ICU are safe because we found that less than 3% of all physical therapy interventions observed resulted in adverse events evolving with some damage, and most physiological abnormalities or adverse events were near miss and did not result in an increased length of ICU or hospital stay. There were no falls, accidental extubation, and loss of associated devices, which are described as rare during physical therapy interventions.12,13 All these findings are consistent with those found in previous studies with mixed populations.12,13,26
In our secondary analysis to explore the relationship between the occurrence of physiological abnormalities or adverse events with patients’ baseline characteristics, only the presence of comorbidities was associated with occurrence of these events. Pre-existing hypertension was one of the most common comorbidities and its impact is well established on surgical patient outcome. Systematic reviews and meta-analysis have shown that hypertension increased perioperative complications and is associated with major adverse events and 30-day mortality after surgery.31,32
We did not find differences between clinical outcomes of patients with or without physiological abnormalities or adverse events. A possible explanation for this result is that the majority of events were detected before they evolved to harm or loss of function. Sricharoenchai et al.13 observed that patients with potential safety events had a longer length of ICU and hospital stay, but they reported that this is more likely because these patients have a greater opportunity to receive more physical therapy interventions and, thus, higher risk for an event, and may also have a greater severity of illness and medical instability. Even though the occurrence of these events was not associated with worse clinical outcomes, we believe physical therapists working in this scenario need to develop strategies to improve patient safety.
Our study has some limitations. First, it was performed at a single center; therefore, the occurrence of physiological abnormalities or adverse events may have been influenced by the center's practice. However, we believe our results may be generalizable to similar surgical ICUs with patients with severe clinical conditions. Secondly, we observed each type of physical therapy intervention once per patient during ICU stay to ensure study feasibility, so that the incidence of adverse events we reported is the incidence during observed events and does not include all physical therapy interventions, and some interventions were observed only a few times, such as walking and nasotracheal suctioning. But to increase the reliability of our results, we calculated the 95% CI of the observed incidence, and to minimize selection bias we observed always the first time that the intervention was used.
And finally, it is an observational study, and as a consequence, we cannot make any conclusions about cause and effect, or be sure that all bias was avoided. To minimize bias, we chose to use very broad inclusion criteria, collected all data prospectively, and measured our outcomes in a very objective manner.
This study also has several strengths. First, we used well described definitions of our outcomes. Second, we measured the incidence of physiological abnormalities or adverse events prospectively by direct observation, reducing misreporting. Third, the study was performed in an ICU with low mortality where certified intensivists and physical therapists manage patients 24 h a day, 7 days a week. Finally, to know the incidence of physiological abnormalities or adverse events and factors associated with these events will help us prevent the occurrence of such events and increase patient safety.
ConclusionThe incidence of physiological abnormalities or adverse events was 20% during physical therapy interventions in patients after cardiac surgery in the ICU, especially in those undergoing invasive MV, but most of them were near miss and required minimal to no additional treatment. The presence of comorbidities was associated with physiological abnormalities or adverse events, but the occurrence of these events was not associated with worse clinical outcomes.
Sources of fundingNo funding was received for this study.
Trial registration number: NCT03552887 (https://clinicaltrials.gov/ct2/show/NCT03552887)