Modifications of posture in a segment may influence the posture of adjacent and nonadjacent segments and muscular activity. The spine–shoulder and spine–pelvis relationships suggest that the pelvis may influence shoulder posture.
ObjectiveTo investigate the effect of the active reduction of the anterior pelvic tilt on shoulder and trunk posture during static standing posture and on the electromyographic activity of the scapular upward rotators during elevation and lowering of the arm.
MethodsThirty-one young adults were assessed in a relaxed standing position and a standing position with 30% active reduction of the anterior pelvic tilt. The pelvic tilt, trunk posture, and forward shoulder posture during the static standing posture and the electromyographic activity during elevation and lowering of the arm were assessed.
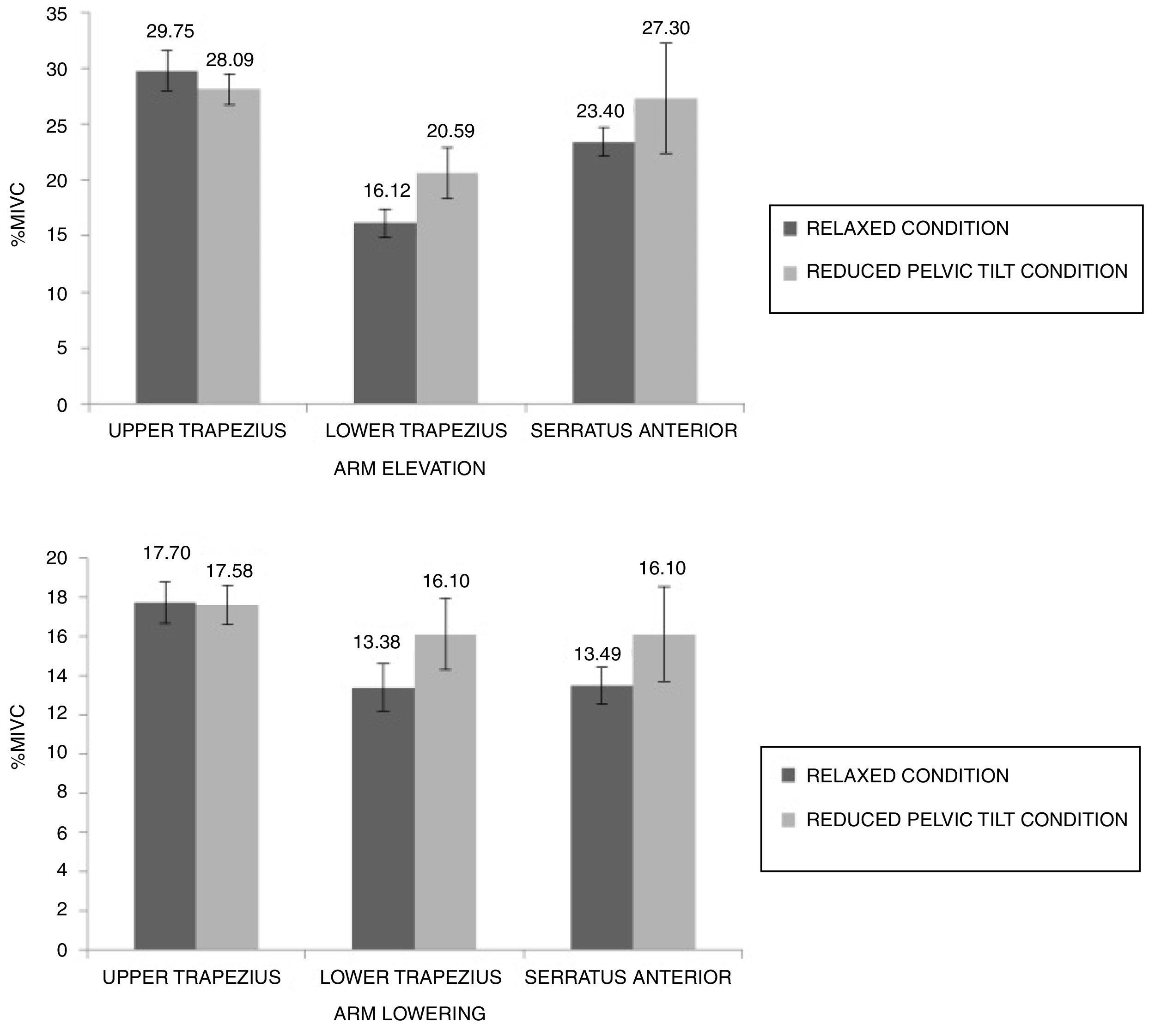
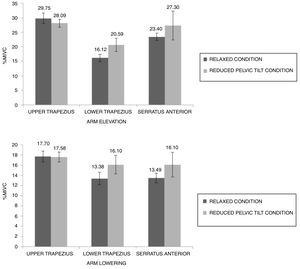
ResultsPaired t-tests indicated that the active reduction of the anterior pelvic tilt reduced the trunk extension (MD=1.09; 95%CI=−2.79 to −1.03). There were no effects on the forward shoulder posture (MD=0.09; 95%CI=−0.92 to 1.09). Repeated measures of analyses of variance indicated an increase in lower trapezius electromyographic activity (MD=3.6; 95%CI=1.28 to 5.92). There was a greater reduction in upper trapezius activity after pelvic tilt reduction during arm elevation (MD=1.52%; 95%CI=−2.79 to −0.25) compared to that during the lowering phase. There were no effects of pelvic tilt reduction on the electromyographic activity of the serratus anterior (MD=3.26; 95%CI=−3.36 to 9.87).
ConclusionThe influence of pelvic posture on the trunk posture and lower trapezius activation should be considered when assessing or planning exercise for individuals with shoulder or trunk conditions.
The presence of a forward shoulder posture, reduced scapular upward rotation and alterations in electromyographic (EMG) activity of the scapular upward rotators muscles have been related to shoulder dysfunctions.1,2 Interventions aiming to improve shoulder and scapula alignment by means of changing soft tissue properties around the shoulder, such as stretching of the pectoralis minor3 and major and strengthening of the scapular upward rotators muscles,4,5 have been proposed. However, the effects of these exercise programs on shoulder posture are contradictory. A possible reason for the absence of effects observed in some studies could be that they do not consider the influence of nonadjacent segments on shoulder posture during the intervention.
In upright posture, the posture of a body segment can be influenced by the posture of nonadjacent segments.6 Considering this, spinal posture may influence the shoulder complex posture.7 More specifically, increased thoracic kyphosis increases the scapular anterior tilt and internal rotation, which are components of forward shoulder posture,7 and it alters the EMG activity of the scapular upward rotators muscles.8 This spine–shoulder relationship may be related to tissue connections between the shoulder, scapula and thoracic spine.7 Spinal posture is also related to pelvic posture.6,9 Specifically, an increase in the anterior pelvic tilt is associated with increased lumbar lordosis,6,9 which is related to increased thoracic kyphosis.9 Therefore, modifications in pelvic posture may influence the shoulder complex posture through changes in spinal posture.
Spinal and shoulder postures may also influence the scapular position and EMG activity of muscles during different arm movements.10 Alterations in scapular position may modify the length-tension relationship of the trapezius and serratus anterior (SA) and, consequently, change their activity during elevation and lowering of the arm. Previous studies have demonstrated that individuals with forward shoulder posture have lower SA activity11 and a higher upper trapezius (UT) during arm lift movements compared to healthy individuals.12 Furthermore, the reduction in forward shoulder posture increases the activity of the lower trapezius (LT) during shoulder flexion.13 Thus, modifications in pelvic posture may influence the activity of the scapular muscles by modifying the spinal and shoulder complex postures.
Therefore, the purpose of this study was to investigate the effects of active reduction in the anterior pelvic tilt on shoulder and trunk postures during static standing and on the activity of the scapular upward rotators during elevation and lowering of the arm in the frontal plane. We hypothesized that a reduction in the anterior pelvic tilt would reduce forward shoulder posture, reduce UT activity and increase SA and LT activity during arm elevation.
Material and methodsParticipantsThirty-one healthy individuals participated in this study (12 males and 19 females), and they had a mean age of 25.81±3.28 years, a mean body mass of 64.64±9.96kg, a mean height of 1.69±0.10m and a mean body mass index of 22.66±2.18kg/m2. The eligibility criteria were as follows: age between 18 and 35 years; presence of forward shoulder posture; body mass index equal to or less than 28kg/m2; no injuries in the last three months; no history of pelvic, spinal or upper limb surgeries; and able to reduce at least 30% of the anterior pelvic tilt. Forward shoulder posture was identified using a posture assessment grid and defined as anterior displacement of the middle point between the anterior and posterior borders of the acromion of the dominant shoulder in relation to a vertical reference line aligned to the lateral malleoli and greater femoral trochanter.14 Participants with severe pelvic posterior inclination, reduction of lumbar lordosis or severe thoracic kyphosis were excluded from this study. Participants signed informed consent prior to participating in this study, that was approved by the research ethics committee of the Universidade Federal de Minas Gerais, Belo Horizonte (UFMG), Minas Gerais, Brasil (number 30883114.3.00005149).
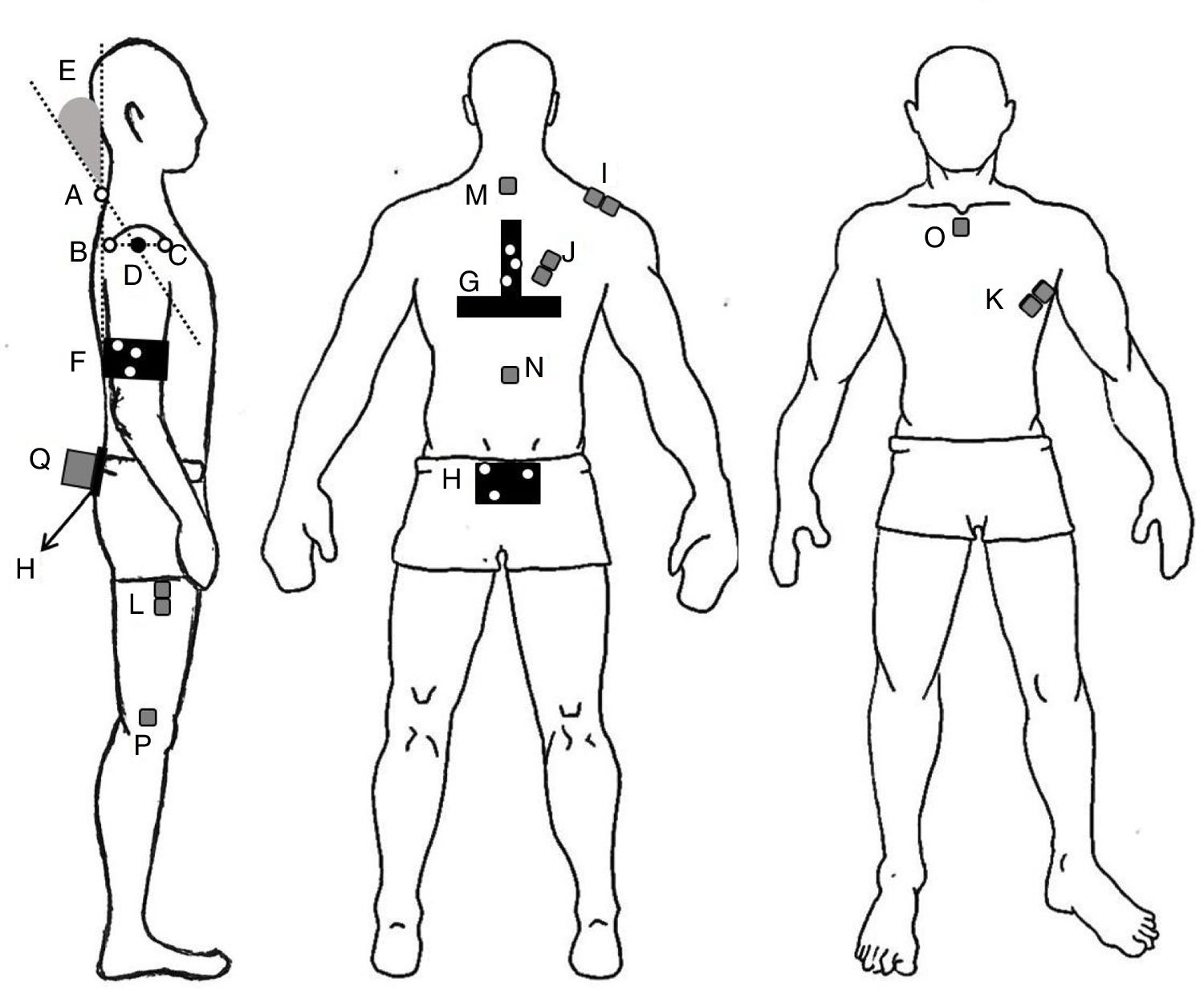
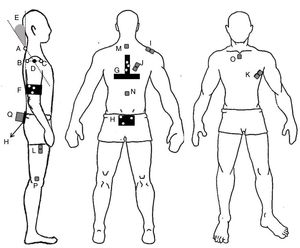
ProceduresThe procedures included an assessment of the shoulder, trunk and pelvis static posture and the measurement of EMG activity of the scapular upward rotators during arm elevation and lowering. The participants performed underwent the assessment in two experimental conditions: a habitual standing position (hereafter referred to as the relaxed condition) and a standing position with 30% active reduction of the anterior pelvic tilt (hereafter referred to as the reduced pelvic tilt condition). In a pilot study, we tested different magnitudes of pelvic tilt reduction and found that 30% reduction was sufficient to induce significant changes in pelvic tilt without reaching extreme retroversion of pelvic posture. We used the magnitude of the pelvic tilt of each participant obtained during the relaxed condition to define the 30% reduction in the anterior pelvic tilt in the reduced pelvic tilt condition. The pelvic position during data collection was double-checked. First, with a digital inclinometer (Protractor Pro 3600®) positioned on the sacrum15 (Fig. 1), the examiner monitored if the individual performed the pelvic tilt reduction as oriented and if there was no change to the pelvic posture during the trial. After each trial, the pelvic posture was checked in Visual 3D software (C-Motion Inc., Germantown, MD, United States) using the data collected by the motion capture system. Trials in which the participant did not maintain the correct pelvis position were discarded, and the procedure was repeated. A variation of two degrees in the pelvic position was allowed. Only trials with the correct reduction of pelvic position were considered for inclusion in the analyses.
Setup of the active markers, clusters, electromyography electrodes, inclinometer and forward shoulder posture calculation. Active markers placed on the spinous process of the C7 (A); posterior (B) and anterior (C) borders of the acromion; the middle point between the anterior and posterior borders of the acromion (D). Forward shoulder posture angle (E). Clusters placed on the arm (F), trunk (G), and sacrum (H). EMG electrodes placed on the upper trapezius (I); lower trapezius (J); and serratus anterior (K); electrode placed on the thigh (L); reference EMG electrodes placed on the spinous process of T2 (M) and T10 (N), on the manubrium of the sternum (O), and on the lateral condyle of the femur (P); inclinometer placed over the sacrum (Q).
The Codamotion analysis system (Charnwood Dynamics Ltd., Tothley, Leics., England) was used to capture the body segment postures and arm movement at a sample rate of 100Hz. Active markers were placed on the anterior and posterior borders of the acromion and on the spinous process of the seventh cervical vertebrae (C7) to measure the shoulder posture11 (Fig. 1). We positioned a cluster with three noncollinear active markers between the scapulae to track the trunk posture and over the midpoint between the posterior superior iliac spine to track the pelvic posture. To track the arm during elevation and lowering, we positioned a cluster on the dominant arm at 3cm above the lateral humeral epicondyle. The following anatomical markers were identified to later create the biomechanical model: both acromia and iliac crests to define the trunk, the iliac crests and femoral trochanters to define the pelvis, and the acromion and medial and lateral humeral epicondyles to define the arm.16
The EMG signal was registered using the ME 6000 (MegaEletronics, Kuopio, Finland) at a sample rate of 1000Hz. Pairs of active surface circular electrodes were placed 2cm apart over the muscle belly of the dominant UT (halfway between the C7 and the acromion), SA (immediately below the axillary area at the level of the inferior tip of the scapula and just medial to the latissimus dorsi) and LT (approximately 5cm lower than the scapular spine at an oblique angle) (Fig. 1) along the line of the muscle fibers.17 Before each electrode was placed, the skin surface was shaved and cleaned with alcohol to minimize skin impedance.17 The reference EMG electrodes were placed on the spinous processes of T2 and T10, on the manubrium of sternum, and on the lateral condyle of the femur (Fig. 1). In addition, a pair of electrodes was placed on the thigh of the participant to allow for synchronization between the EMG and the kinematic data. The same investigator conducted all of the preparations for all of the participants. The procedures used in the EMG evaluation were conducted in accordance with current recommendations of the International Society of Electrophysiology and Kinesiology.
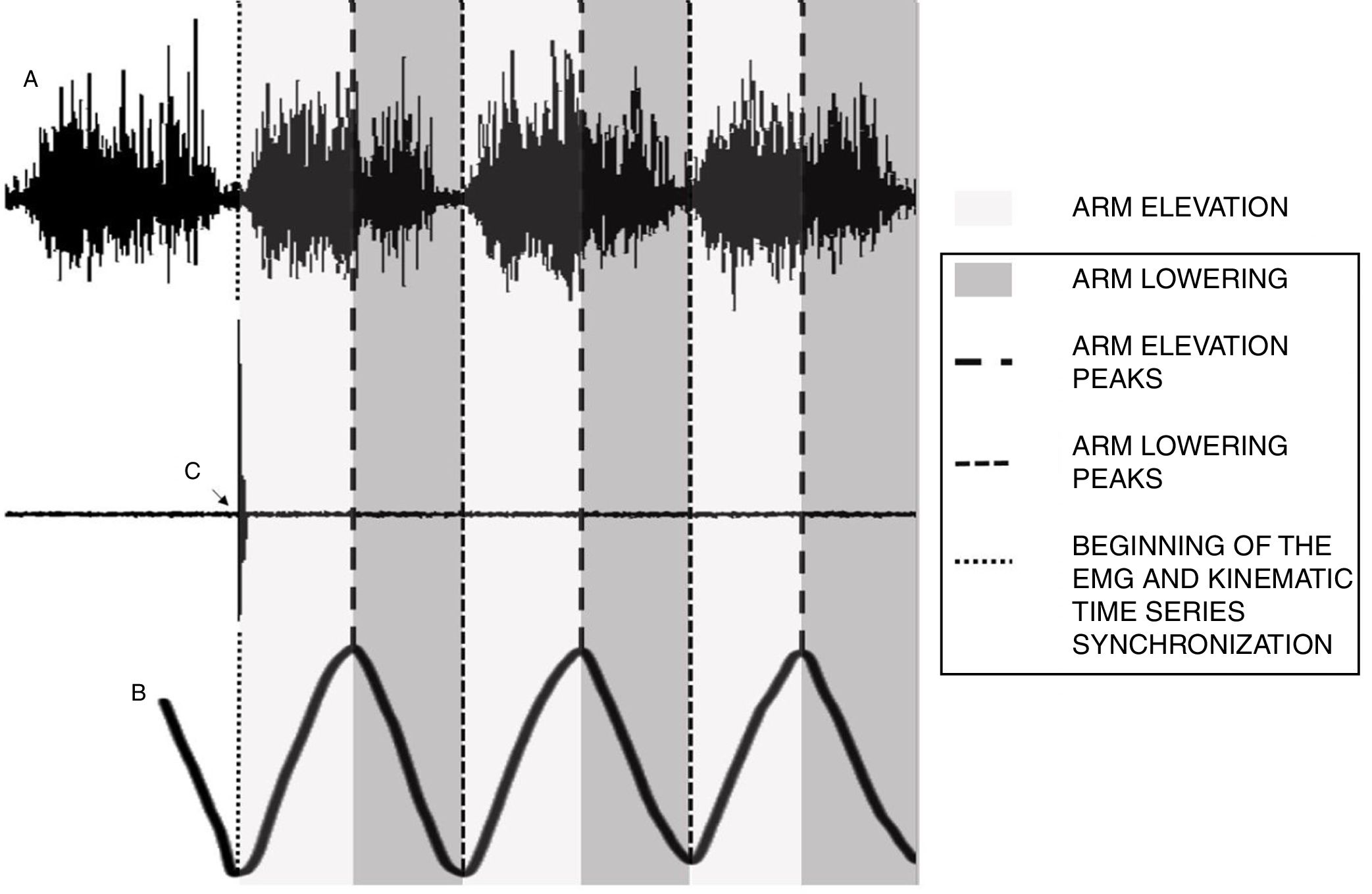
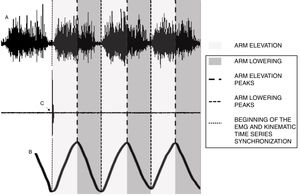
Three trials, each lasting 5s, in a static posture position were recorded to quantify the postures of shoulder, trunk and pelvis. Afterwards, to verify the effect of pelvic tilt reduction on EMG activity of the scapular upward rotators, the participants were trained to elevate and lower the arm in the frontal plane in synchrony with a metronome (M&M System, Lich, Germany). Five minutes of rest were given to them if they did not synchronize with the metronome after ten attempts. After synchronization with the metronome was achieved, the participants were instructed to perform six repetitions of arm elevation and lowering, touching the thigh electrode on the second repetition of each trial. Three trials of six repetitions were carried out, and 3min of rest were given between trials. The moment of the signal peak registered by the thigh electrode was used to cut the EMG and kinematic time series.
After data collection in the relaxed condition was performed, we repeated the same procedures for the reduced pelvic tilt condition. Before data collection was performed, each participant was trained to change and sustain the pelvic position. Only after this familiarization procedure was taught did we perform the evaluation in the relaxed pelvic position followed by that in the reduced pelvic tilt condition.
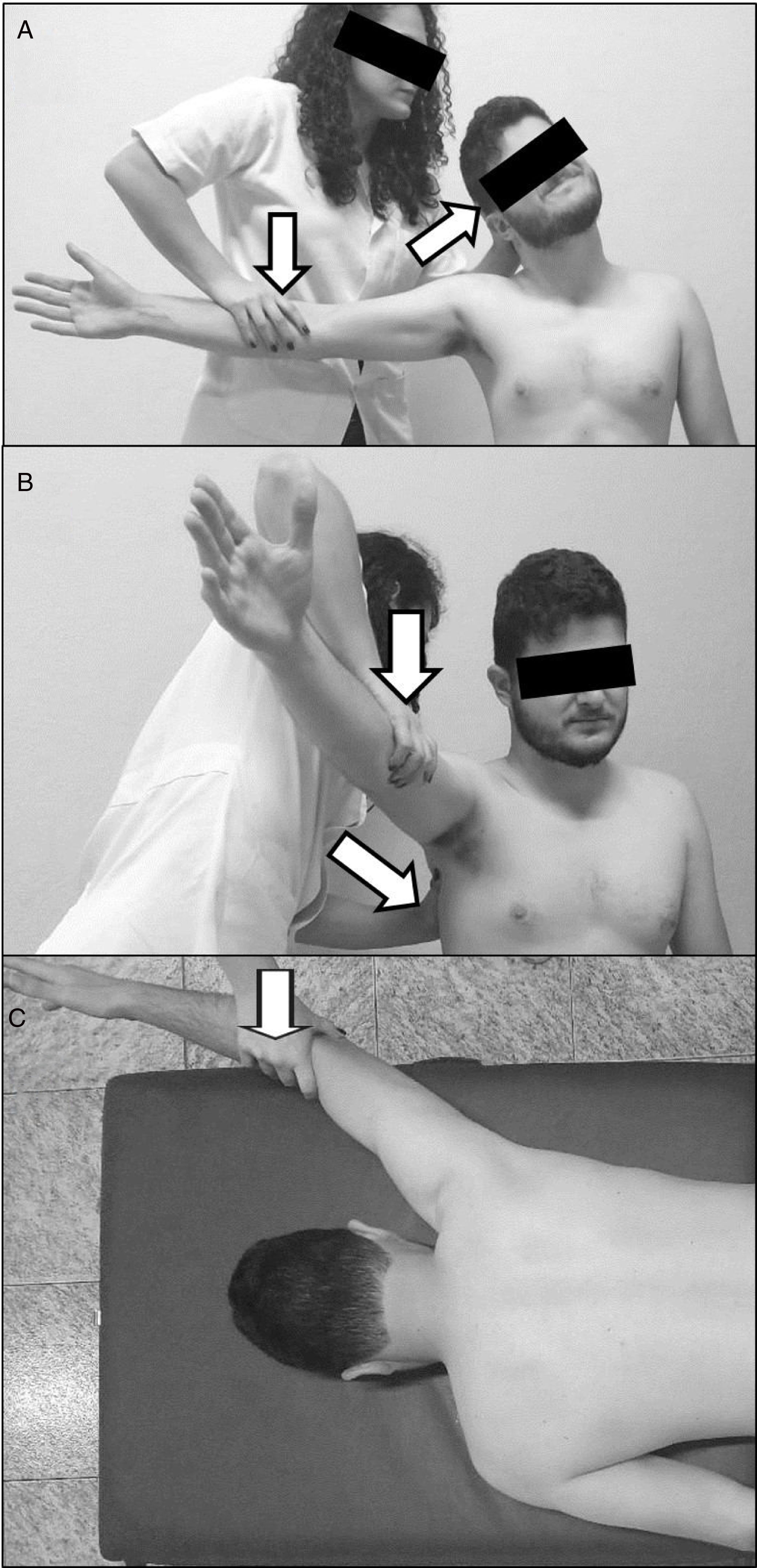
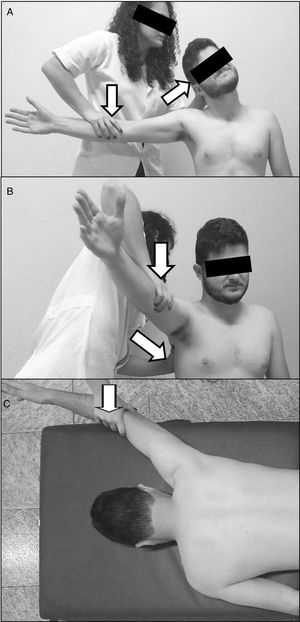
At the end of the data collection, the participants carried out three repetitions, 5s each, of the maximum voluntary isometric contraction (MVIC) of each muscle to normalize the EMG signal collected during arm elevation and lowering.18 For MVIC of the upper trapezius, with the shoulder abducted, neck side-bent to the same side and rotated to the opposite side, the individual resisted the examiner's force applied on head and elbow (Fig. 2A). For serratus anterior MVIC, with the shoulder abducted in the plane of the scapula, the individual resisted the examiner's force applied above the elbow and at the inferior angle of the scapula (Fig. 2B). To assess MVIC of the lower trapezius, in prone position with an arm raised above the head in line with the lower trapezius muscle fibers, the individual resisted the examiner's force applied above the elbow (Fig. 2C).
The same examiner trained in all measurement procedures performed the measures in a motion analysis lab. A pilot study with nine subjects demonstrated that the posture and EMG activity measurements had excellent test–retest reliability. More specifically, in the relaxed position, the pelvic tilt, trunk, pelvis and shoulder postures produced intraclass correlation coefficients (ICC3,2) and standard error of measurements (SEM) of 0.83 (2.84°), 0.96 (2.25°), 0.96 (2.27°), and 0.94 (2.10°), respectively. The ICC (SEM) for the EMG variables in this condition were 0.91 (3.15%), 0.99 (1.20%), and 0.87 (3.93%) for UT, LT and SA, respectively. In the reduced pelvic tilt condition, the ICC (SEM) were 0.86 (1.91°), 0.96 (2.49°), 0.96 (2.06°) and 0.93 (2.10°) for the pelvic tilt, trunk, pelvis and shoulder postures, respectively. The ICC (SEM) for the EMG variables in this condition were 0.89 (3.37%), 0.98 (1.32%), and 0.92 (2.87%) for UT, LT and SA, respectively.
Data reductionThe forward shoulder posture was measured as the planar angle between a line connecting C7 marker with the midpoint of the dominant acromion and a vertical line (Fig. 1).11 We defined the posture of the trunk and pelvis in the sagittal plane as the position of these segments relative to the laboratory (medial–lateral axis). Negative values indicated trunk extension and a posterior pelvic tilt. Positive values indicated trunk flexion and an anterior pelvic tilt. We used the Visual 3D software (C-Motion Inc., Germantown, MD, United States) to process the data. The mean values of the three trials in each condition were considered for the analyses.
A MATLAB (Mathworks, Inc., Massachusetts, United States) code was used to process the EMG and kinematic data. The signal registered by thigh electrode corresponded to the lowest amplitude of the lowering arm movement, and it was used to cut the EMG and kinematic time series to be processed for further analysis. Therefore, the EMG and kinematic registration of the first repetition before the signal peak of the thigh electrode (second repetition) was discarded, and only EMG data corresponding to the subsequent arm elevation and lowering after the signal peak of the thigh electrode (five subsequent repetitions) were processed (Fig. 3). The EMG signals were full-wave rectified and subsequently filtered with a Butterworth bandpass filter with cutoff frequencies of 30 and 500Hz. We used the highest value of the root mean square (RMS) of the signals of each muscle during the MVIC to normalize the EMG signals during minimum arm lowering and maximum elevation angles (arm elevation) and during maximum arm elevation and minimum lowering angles (arm lowering). The highest and lowest EMG obtained in the five arm movement repetitions were discarded, and we used the trimmed mean values of the three trials of the normalized EMG activity of each muscle during arm elevation and lowering in each condition for the statistical analyses.
Synchronization procedure of electromyography (EMG) and kinematic time series. (A) EMG signal recorded during arm elevation and lowering; (B) arm angular displacement; and (C) instant of occurrence of the thigh electrode signal peak, which was used to cut the EMG and kinematic time series.
As all variables were normally distributed, paired t-tests were used to investigate the differences between the two conditions (relaxed position vs reduced pelvic tilt) in regards to their effect on the postures of shoulder, trunk and pelvis. The effect sizes were obtained using GPower software. Repeated measures analyses of variance (ANOVA) with two within-subject effects, pelvic tilt (relaxed and reduced pelvic tilt conditions) and phase of movement (arm elevation and lowering), were used to investigate the main effect of the pelvic tilt condition and to investigate if this effect was dependent on movement phases (interaction effect). To explore the interaction effect, a paired t-test was performed to compare the change (score difference) in EMG activity due to pelvic tilt reduction between movement phases. All analyses were performed with α set at 0.05.
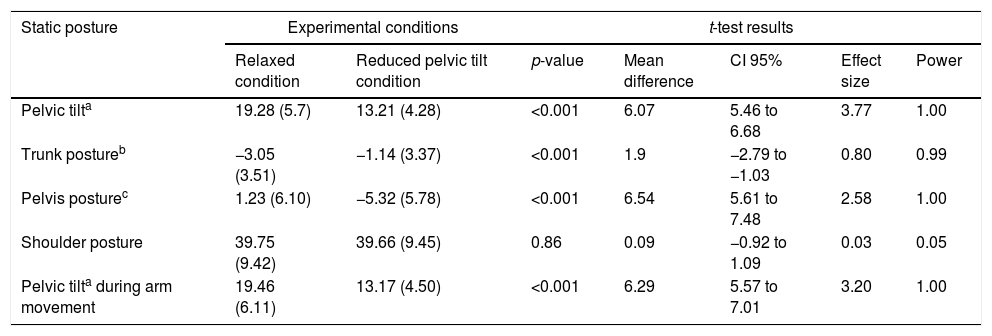
ResultsTable 1 shows the results of the comparisons between the two conditions. During the reduced pelvic tilt condition, the participants demonstrated a 31.48% (SD=4.9%) and 32.32% (SD=5.9%) reduction in the anterior pelvic tilt during elevation and lowering of the arm, respectively, in comparison to the relaxed condition. The mean reduction in the anterior rotation of the pelvis of 6.55° (SD=2.56°) observed in 3D analysis confirms that the active reduction in the anterior pelvic tilt monitored by means of the inclinometer was able to induce changes in pelvic posture to test the hypotheses of this study.
Mean (standard deviation) of pelvic tilt, trunk, pelvis and shoulder posture (in degrees), and the normalized EMG activity (in %).
| Static posture | Experimental conditions | t-test results | |||||
|---|---|---|---|---|---|---|---|
| Relaxed condition | Reduced pelvic tilt condition | p-value | Mean difference | CI 95% | Effect size | Power | |
| Pelvic tilta | 19.28 (5.7) | 13.21 (4.28) | <0.001 | 6.07 | 5.46 to 6.68 | 3.77 | 1.00 |
| Trunk postureb | −3.05 (3.51) | −1.14 (3.37) | <0.001 | 1.9 | −2.79 to −1.03 | 0.80 | 0.99 |
| Pelvis posturec | 1.23 (6.10) | −5.32 (5.78) | <0.001 | 6.54 | 5.61 to 7.48 | 2.58 | 1.00 |
| Shoulder posture | 39.75 (9.42) | 39.66 (9.45) | 0.86 | 0.09 | −0.92 to 1.09 | 0.03 | 0.05 |
| Pelvic tilta during arm movement | 19.46 (6.11) | 13.17 (4.50) | <0.001 | 6.29 | 5.57 to 7.01 | 3.20 | 1.00 |
The reduced pelvic tilt condition resulted in a less extended trunk posture. However, there were no differences in shoulder posture (Table 1). Regarding the LT activity, a main effect of the pelvic tilt condition (F=10.04; p=0.004; η2=0.251; Power=0.865) and an interaction effect (F=7.08; p=0.01 η2=0.191; Power=0.731) were observed. The reduction in anterior pelvic tilt increased the LT activity in both movement phases, but this increase was more pronounced during the elevation movement (t=2.66; p=0.012; effect size=0.48; Power=0.73). For the UT activity, there was no pelvic tilt condition effect (F=1.85; p=0.18; η2=0.058; Power=0.261). However, an interaction effect was observed (F=5.96; p=0.02; η2=0.166; Power=0.656), indicating a reduction of UT activity during arm elevation (reduction of 1.65%) compared to the lowering movement (reduction of 0.12%) (t=−2.41; p=0.021; effect size=0.44; power=0.66). Regarding SA activity, no main effect of the pelvic tilt condition (F=1.01; p=0.32; η2=0.033; Power=0.164) or interaction effect (F=0.28; p=0.59; η2=0.01; Power=0.081) was observed. The results of the EMG activity are presented in Fig. 4.
DiscussionThis study investigated the effects of active reduction of the anterior pelvic tilt on the shoulder and trunk postures during the static posture position and on the EMG activity of the scapular upward rotators during arm elevation and lowering. The results demonstrate that the reduction in anterior pelvic tilt resulted in a less extended trunk posture and an increased LT EMG activity during both arm elevation and lowering. In addition, we observed that reduction of the pelvic tilt reduced the UT activity, but this was only true in the elevation phase. There were no differences in forward shoulder posture and SA EMG activity between before and after active reduction of the anterior pelvic tilt.
The less extended trunk posture observed after the reduction in the anterior pelvic tilt suggests interaction between the spine and the pelvis, as previously reported.6,9 The reduction in anterior pelvic tilt may have posteriorly displaced the body's center of mass. Therefore, to maintain the projection of the body's center of mass as being centered in the anteroposterior direction of the body base of support,19 the individuals reduced their extended trunk posture and, consequently, anteriorly displaced the projection of the body's center of mass. Therefore, the change in trunk posture after reduction of the anterior pelvic tilt could be a strategy to maintain a better alignment relative to the gravity line. Although a statistically significant difference was observed, the clinical relevance of the trunk posture change needs to be discussed.
Although a difference of 0.7° could be considered minimally important according to calculation proposed by Lemieux et al.,20 the small magnitude of change in trunk posture may not be clinically important due to the high variability of this measure. In this sense, future studies testing major magnitudes of pelvic tilt reduction may observe more meaningful changes in trunk posture.
Change in forward shoulder posture was not observed after reduction of the anterior pelvic tilt was performed. One explanation for this result is that the posture of a joint depends not only on the alignment of adjacent segments6 but also on the properties (e.g., resting length) of the muscles around this joint.21 Individuals with forward shoulder posture often present with shorter pectoralis minor1,22 and major14 resting muscle lengths and posterior shoulder tightness.22,23 In this sense, this short muscle resting length may resist changes in pelvic posture and thus hamper the reduction in the anterior shoulder posture. In addition, the high variability in spine alignment in the sagittal plane (i.e., different magnitudes of lumbar lordosis and thoracic kyphosis) demonstrated by a previous study24 may have hampered the effects of pelvic posture on trunk and shoulder postures. Thus, the investigation of how tissue characteristics around the shoulder and the alignment of the spine would influence changes in posture in future studies may improve understanding of the possible effects of pelvis posture on shoulder posture.
The active reduction in the anterior pelvic tilt increased the LT EMG activity during arm movement. Specifically, an increase of 4.47% in LT EMG after pelvic tilt reduction during arm elevation and an increase of 2.81% during arm lowering were observed. Although these values are apparently small, they are greater than the SEM, and there is evidence that muscular activation level of 2.9% can offer increased protection to the joints.25 In addition, considering the minimally important difference calculation proposed by Lemieux et al.,20 a difference of 1.37% could be considered a relevant difference for this variable.20 A possible explanation for the increase in LT activation is that, in the reduced pelvic tilt condition, the subjects might have recruited the gluteus maximus to perform and maintain the reduced pelvic tilt position. The gluteus maximus contraction tightens the thoracolumbar fascia, which may destabilize/move the scapula, resulting in activation of the LT.26 This argument is reinforced by evidence of an increase in LT activity during exercises involving gluteus maximus contration.26 Alternatively, or in addition to, the participants likely increased their abdominal muscle contraction to reduce the pelvic anterior tilt. Therefore, given that conscious contraction of the abdominal muscles increases the EMG amplitude in the scapular muscles, including the LT EMG amplitude,27 increased abdominal muscle contraction may help to explain the increased LT activity. This possibility is a secondary hypothesis since there were no effects of this on SA activity.
In addition to effects of reduced anterior pelvic tilt on LT EMG activity, there was a reduction of the UT activity only during arm elevation. Although this reduction was statistically significant, the reduction of 1.65% observed during arm elevation, compared to reduction of 0.12% during lowering movement, is below the SEM and therefore may not be clinically significant. The low effect size obtained for the main effect of pelvic tilt condition for UT and SA suggests the absence of a direct effect of the anterior pelvic tilt reduction on the EMG activity of these muscles. The more superior insertions of the UT and SA may make them more dependent on changes in the cervical, scapular, shoulder and rib cage posture, which are findings that were not demonstrated nor investigated in this study. For example, it has been demonstrated that stretching of the pectoralis minor may increase the activity of UT and SA during the execution of the scapular posterior tilt exercise,28 suggesting a possible influence of a shortened/rigid pectoralis minor on the activity of these muscles. Future studies should investigate the effects of reduction of the pelvic anterior tilt on the posture of these segments, which may help to explain the lack of an effect of pelvic posture on SA and UT activity.
In the present study, the average reduction in the anterior pelvic tilt was 6°. Based on data published in the literature, the difference between the normal pelvic position and the maximum posterior pelvic tilt is approximately 6° to 8°.15,29 Therefore, the reduction in the anterior pelvic tilt induced in the present study could not be considered small in magnitude since the values are similar to the maximum posterior pelvic tilt values reported in the literature. A number of the participants may have lacked an increase in the anterior pelvic tilt posture, which is a possible limitation of this study. However, there are no reference angle values for excessive posterior pelvic tilt (pelvic retroversion) or excessive anterior pelvic tilt (pelvic anteversion) to date based on inclinometer or 3D measures. Individuals with increased anterior pelvic tilt may respond differently to a reduction in the pelvic tilt. For example, these individuals may demonstrate effects on the shoulder posture and on SA and UT activity, which are findings that were not demonstrated in this study. In addition, defining the trunk as a single rigid segment was another limitation to the present study since identifying the changes that were specifically related to the thoracic spine (i.e., independent of the lumbar spine) was not possible. Finally, different methods to measure the forward shoulder posture are described in the literature,5 and the use of these could lead to different results.
The results of the present study suggest that active reduction of the pelvic anterior tilt increases LT EMG activity during arm elevation. Our results reinforce the finding regarding the interaction between the pelvis and trunk segments and demonstrate that, although no changes were observed in shoulder posture, active changes in pelvic posture may influence scapular muscle activation, and more specifically, that in the LT muscle. Considering this result, the modification of pelvis posture might be used to increase LT EMG activity during rehabilitation programs for individuals with shoulder conditions, such as subacromial pain and impingement syndromes, which can be associated with diminished activity of the LT muscle.30,31 However, the modification of pelvis alignment and its effects on LT EMG activity in these clinical populations needs to be investigated further.
ConclusionsActive reduction of 30% in the anterior pelvic tilt resulted in a less extended trunk, and it increased LT EMG activity. The reduction of UT activity observed during arm elevation may be not clinically relevant. In addition, reducing the pelvic anterior tilt did not modify the shoulder posture or the SA EMG activity.
Conflicts of interestThe authors declare no conflicts of interest.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES - Finance Code 001). We are also thankful to the State of Minas Gerais Funding Agency FAPEMIG (APQ-02427-15) and to the Brazilian Funding Agency CNPQ.