To determine the immediate effects of a varus unloader knee brace on lower-limb electromyographic activity in individuals with lateral knee osteoarthritis and valgus malalignment after anterior cruciate ligament reconstruction.
MethodsElectromyographic data were recorded in 19 individuals with lateral knee osteoarthritis and valgus malalignment after anterior cruciate ligament reconstruction during walking under three conditions: (i) no brace, (ii) unadjusted brace (no varus adjustment), and adjusted brace (varus adjustment). Variables of interest were statistically analyzed using repeated measures analysis of variance.
ResultsThere were no significant differences in muscle co-contraction between the three test conditions. The adjusted brace resulted in delayed offset of gluteus maximus (mean difference [95% CI]: 72ms [24, 119]), and earlier onset of gluteus medius (59ms [21, 97]) compared to no brace. The adjusted brace delayed onset of lateral gastrocnemius compared to no brace (53ms [28, 78]) and the unadjusted brace (39ms [7, 71]) and reduced average activation amplitude of gluteus maximus (−4mV [−6, −1]) and lateral gastrocnemius (−9mV [−16, −2]) compared to no brace.
ConclusionsThe unloader brace did not produce significant changes in muscle co-contraction in individuals with lateral knee osteoarthritis and valgus malalignment after anterior cruciate ligament reconstruction. Significant changes in gluteal and gastrocnemius muscle activation timing and amplitude were observed, however, it is not clear whether these changes are of clinical importance.
Over 50% of individuals 10–20 years following anterior cruciate ligament (ACL) injury show radiographic evidence of knee osteoarthritis (OA).1 Unfortunately, prognosis for knee OA is not improved with ACL reconstruction (ACLR).2 Knee OA after ACLR is associated with considerable knee-related symptoms, functional and psychological impairments, and poorer quality of life than those without knee OA after ACLR.3,4 Importantly, knee OA after ACLR is a condition that is commonly faced by young adults.5
Knee OA can occur in the medial and/or lateral tibiofemoral joint (TFJ) and/or patellofemoral joint (PFJ) compartments. In non-traumatic populations, medial knee OA (i.e., medial TFJ OA with or without PFJ OA) is reported in 56–68% of individuals, while lateral knee OA is only reported in 9–11%.6–8 Thus, it is not surprising that research efforts to date have primarily focused on medial knee OA. However, in individuals with knee OA after ACLR, lateral knee OA is evident in more than 50%.9–11 Given this notably high prevalence of lateral knee OA following ACLR, our previous research has focused on this important subgroup of individuals, and potential differences in treatment aims and mechanisms.
An unloader brace can improve knee pain, confidence and stability in individuals with knee OA after ACLR.12 A varus unloader brace can also modulate lower limb biomechanics in individuals with predominant lateral knee OA after ACLR — increase knee flexion and adduction angles and moments during level walking13 and high-demand activities such as hopping and stair ambulation.14 It has been hypothesized that reductions in knee pain observed in individuals with knee OA with an unloader knee brace could be mediated by muscle activation patterns, which in turn reduces joint load.15 A recent study reported that valgus knee bracing can reduce medial to lateral muscle co-activation in healthy adults.16 Therefore, the current study aimed to investigate the muscle activity response to varus unloader brace in individuals with predominant lateral knee OA after ACLR. Specifically, the aims of this study were to determine the immediate effects of a varus unloader brace on (i) co-contraction of agonist and antagonist muscles, and (ii) timing and amplitude parameters of lower-limb muscles, during level walking in individuals with predominant lateral knee OA after ACLR.
MethodsStudy design and participantsThis within-subject study is an extension of our previous research investigating the effects of a varus unloader brace on lower-limb biomechanics during level walking.13 The recruitment and eligibility criteria have been previously described.13 The primary inclusion criteria were as follows: (i) undergone a primary ACLR (hamstring tendon or patellar tendon graft) five to 20 years ago; (ii) aged ≥16 years at the time of ACLR; and (iii) symptomatic [Knee Injury and Osteoarthritis Outcome Score (KOOS) criteria],17 and radiographic (≥1 grade osteophyte) OA in the lateral TFJ and/or PFJ.18 A trained investigator (KMC) graded TFJ and PFJ disease severity (intra-rater reliability: kappa 0.75–0.84).19 The radiographs in postero-anterior views were used to assess static frontal-plane knee alignment by a trained investigator (intraclass correlation coefficient=0.89), using previously described methods.20 Angles between 178.5° to 180° were defined as neutral alignment, angles <178.5° were defined as varus malalignment, and angles greater than 180° defined valgus malalignment.20 The KOOS consisted of five subscales. A normalized score out of 100 is calculated for each subscale, where 0 represents maximum knee-related symptoms, and 100 represented no knee-related symptoms.21 All participants provided written informed consent prior to data collection. Ethical approval for the study was obtained from The University of Melbourne Human Research Ethics Committee (HREC: 1238328.2).
Acquisition of muscle electromyographic dataMuscle electromyographic (EMG) data presented in the current study were acquired during quantitative gait analyses. Retro-reflective markers were attached at specific locations on participant's pelvis (left/right anterior superior iliac spine, sacral, left/right posterior superior iliac spine) and both lower extremities — thigh (left/right proximal and anterior aspect, proximal and lateral aspect, distal and anterior aspect, distal and lateral aspect), knee (left/right medial and lateral femoral epicondyles), leg (left/right proximal and distal ends of tibia and lateral aspect of tibia), and foot (left/right medial and lateral malleolus, proximal and distal aspects of the posterior calcaneum, dorsal surface of the distal forefoot at the midpoint between the second and third metatarsophalangeal joints, lateral midpoint over the dorsal and distal aspect of the cuboid, medial midpoint over the distal and dorsomedial aspect of the navicular — for gait analyses,22 with thigh and calf markers positioned to accommodate the brace.23 EMG data were recorded at 1080Hz using pairs of Ag/AgCl surface electrodes (Motion Laboratory Systems, Baton Rouge, LA, USA) mounted on the skin over the following muscles: gluteus maximus (GMAX), gluteus medius (GMED), vastus medialis (VM) and vastus lateralis (VL), rectus femoris (RF), medial hamstrings (MHAM), lateral hamstrings (LHAM), medial gastrocnemius (MGAS), lateral gastrocnemius (LGAS) and tibialis anterior (TA) via a telemetered EMG system (Noraxon USA Inc., Scottdale, AZ, USA). Recommendations of the SENIAM group (Surface ElectroMyoGraphy for the Non-invasive Assessment of Muscles) were followed for skin preparation and electrode placement locations.24 The skin surface was shaved, lightly abraded, and cleaned with alcohol prior to surface electrodes placement. It was not necessary to change the electrode locations to accommodate the brace.
Participants performed gait trials under three test conditions at a self-selected speed on a 10-meter level walkway. The following conditions were tested: (i) no brace, (ii) unadjusted brace, with sagittal-plane support and no frontal plane realignment, and (iii) adjusted brace, with sagittal-plane support with varus realignment. The unloader brace is designed to control sagittal and transverse plane rotations associated with ACLR, in addition to correcting frontal plane malalignment. The adjusted brace condition was used to assess the effects of adding varus realignment to the sagittal and transverse plane rotational support. Approximately one and half turns of the maximum three turns varus adjustment was provided. The unadjusted brace condition was used to assess the effects of sagittal and transverse plane support, without frontal plane realignment. Participants performed walking trials without the brace first, followed by the two brace conditions applied in a randomized order. Participants were blinded to the differences between the two brace conditions.
Knee painImmediately following each test, participants rated their average levels of knee pain on 100mm visual analog scales. A score of 0mm indicated no pain and a score of 100mm indicated maximum pain.
Data processingThe retro-reflective marker attached to the heel was labeled and trajectory data were filtered with a low pass, fourth order Butterworth filter (zero lag, 6Hz). Data were exported from Noraxon into a csv file and the EMG data were exported and processed using R statistical software (Version 3.3.2 http://www.R-project.org/). Trials were excluded where EMG data was affected by artifact (visually inspected). After correcting for DC offset, the EMG signal was high-pass filtered (20Hz, 4th order Butterworth) and full-wave rectified. EMG signals were low-pass filtered (50Hz, 4th order Butterworth) for the purpose of onset and offset detection. Criteria for EMG burst onset and offset were established as >15% peak amplitude for ≥10% of the gait cycle and <10% of peak amplitude for ≥10% of the gait cycle, respectively.25 Data collected using a ground-embedded force plate13 were used to establish initial foot contact and foot off, while the traces from the heel trajectory marker were used to establish subsequent foot contact, stance time and stride time. EMG traces were analyzed to establish onset, offset, and duration for each muscle. Muscle co-contraction duration was established by determining onset/offset of antagonistic muscle pairs (e.g. VM and MHAM) and measuring duration of dual activity.26 Mean and peak EMG amplitude activity was also recorded for the burst duration. Each participant's data were averaged over three individual trials for each condition. The investigator analyzing the EMG data was blinded to the test conditions. Variables of interest included onset, offset, duration, average and peak magnitude of GMAX, GMED, VM, VL, RF, MHAM, LHAM, MGAS, LGAS, and TA. Co-contraction indices were calculated for different muscle pairs (i.e., medial and lateral) and groups (i.e., flexors and extensors). The following muscles were evaluated: (i) VM and VL; (ii) MHAM and LHAM; (iii) VM and MHAM; (iv) VL and LHAM; (v) MGAS and LGAS; and (iv) flexors (VM, VL, RF) and extensors (MHAM and LHAM).
Statistical analysisHomogeneity and normality were assessed using Kolmogorov–Smirnov analyses. Repeated measures analysis of variance with Least Significant Difference post hoc evaluations were used to assess differences in variables of interest. Greenhouse–Geisser corrections were applied where assumptions of sphericity were not met. All data were analyzed with the Statistical Package for the Social Sciences (SPSS Statistics Version 23, IBM Cooperation. Armonk, NY), with significance set at 0.05.
ResultsParticipants’ characteristicsThis study included 19 individuals with predominant lateral knee OA (15 [79%] men; mean±SD age 37±7 years; height 1.72±0.06m; body mass 80±10kg; body mass index 27±3kg/m2; 13 hamstring-tendon graft; six patellar-tendon graft) who were 12±4 years post-ACLR with valgus malalignment (187°±3). Participants had mild to moderate knee-related symptoms (KOOS-pain, 79±15; KOOS-symptoms, 74±13; KOOS-activities of daily living, 88±15; KOOS-sports and recreation, 87±15; KOOS-quality of life, 58±23). Thirteen participants (68.4%) had lateral TFJ OA and PFJ OA, 5 participants (26.3%) had PFJ OA without lateral TFJ OA, and 1 participant (5.3%) had lateral TFJ OA without PFJ OA.
There were no statistically significant differences in knee pain during walking (mean VAS: no brace=3±4mm, adjusted brace=8±13mm, and unadjusted brace=5±10mm; p=0.151). There were significant differences in gait speed between no brace (1.46±0.13m/s), adjusted brace (1.43±0.11m/s), and unadjusted brace conditions (1.46±0.14m/s) (p=0.011). Gait speed was slower with the adjusted brace condition relative to the no brace (mean difference [95% confidence interval], p-value: −0.038 [−0.062, −0.013], 0.005) and the unadjusted brace (−0.028 [−0.050, −0.006], p=0.014) conditions.
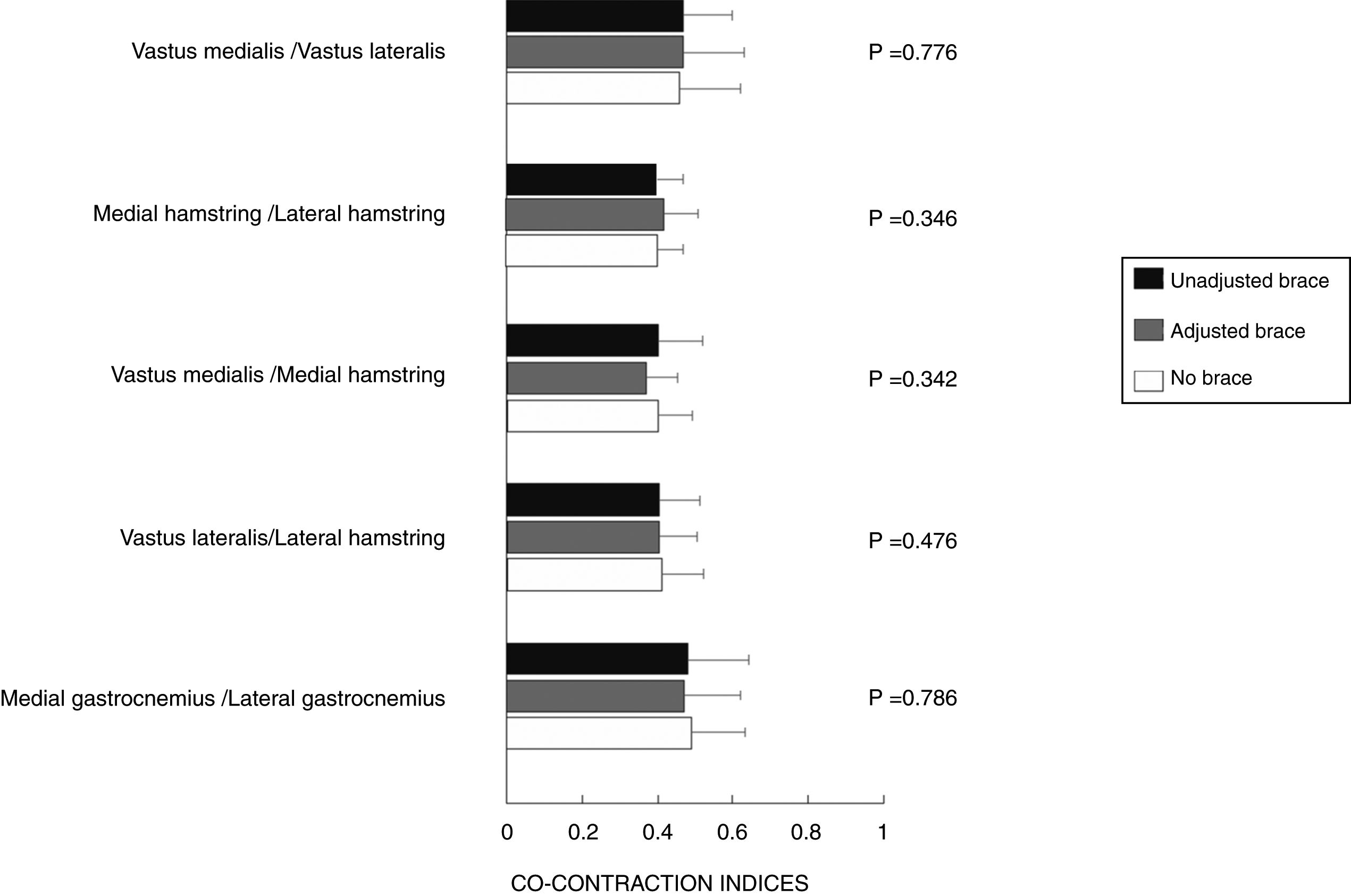
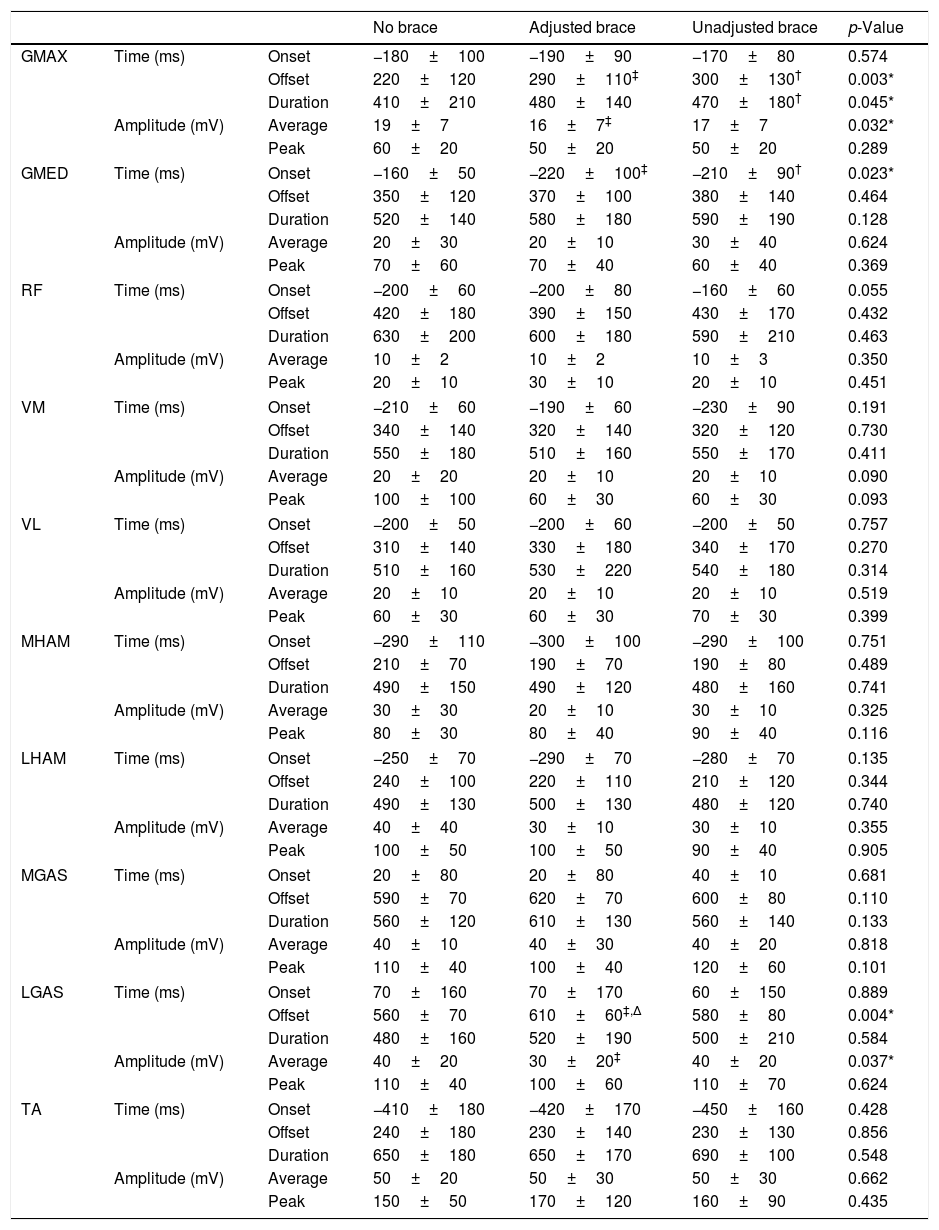
Timing parametersThere were no statistically significant differences in muscle co-contraction between the no brace, adjusted, and unadjusted brace conditions (Fig. 1). There were also no significant differences in co-contraction of flexor-extensor muscle groups (p=0.160).
Relative to the no brace condition, the adjusted (72ms [24, 119], p=0.005) and unadjusted (75ms [24, 126], p=0.007) brace conditions delayed offset time of GMAX (Table 1). The unadjusted brace also significantly increased the duration of GMAX activity compared to no brace (54ms [1, 127], p=0.047); however, differences between no brace and the adjusted brace did not reach statistical significance (p=0.051). Relative to no brace, the adjusted and unadjusted brace conditions resulted in earlier onset of GMED (59ms [21, 97], p=0.004; 43ms [5, 82], p=0.030; respectively). There were no statistically significant differences in GMAX and GMED timing between the two brace conditions. The adjusted brace resulted in delayed offset of LGAS compared to no brace (53ms [28, 78], p<0.001) and the unadjusted brace (39ms [7, 71], p=0.020). There were no other statistically significant differences observed in timing between the three test conditions (Table 1).
Electromyographic parameters during walking for no brace, adjusted brace and unadjusted brace conditions.
| No brace | Adjusted brace | Unadjusted brace | p-Value | |||
|---|---|---|---|---|---|---|
| GMAX | Time (ms) | Onset | −180±100 | −190±90 | −170±80 | 0.574 |
| Offset | 220±120 | 290±110‡ | 300±130† | 0.003* | ||
| Duration | 410±210 | 480±140 | 470±180† | 0.045* | ||
| Amplitude (mV) | Average | 19±7 | 16±7‡ | 17±7 | 0.032* | |
| Peak | 60±20 | 50±20 | 50±20 | 0.289 | ||
| GMED | Time (ms) | Onset | −160±50 | −220±100‡ | −210±90† | 0.023* |
| Offset | 350±120 | 370±100 | 380±140 | 0.464 | ||
| Duration | 520±140 | 580±180 | 590±190 | 0.128 | ||
| Amplitude (mV) | Average | 20±30 | 20±10 | 30±40 | 0.624 | |
| Peak | 70±60 | 70±40 | 60±40 | 0.369 | ||
| RF | Time (ms) | Onset | −200±60 | −200±80 | −160±60 | 0.055 |
| Offset | 420±180 | 390±150 | 430±170 | 0.432 | ||
| Duration | 630±200 | 600±180 | 590±210 | 0.463 | ||
| Amplitude (mV) | Average | 10±2 | 10±2 | 10±3 | 0.350 | |
| Peak | 20±10 | 30±10 | 20±10 | 0.451 | ||
| VM | Time (ms) | Onset | −210±60 | −190±60 | −230±90 | 0.191 |
| Offset | 340±140 | 320±140 | 320±120 | 0.730 | ||
| Duration | 550±180 | 510±160 | 550±170 | 0.411 | ||
| Amplitude (mV) | Average | 20±20 | 20±10 | 20±10 | 0.090 | |
| Peak | 100±100 | 60±30 | 60±30 | 0.093 | ||
| VL | Time (ms) | Onset | −200±50 | −200±60 | −200±50 | 0.757 |
| Offset | 310±140 | 330±180 | 340±170 | 0.270 | ||
| Duration | 510±160 | 530±220 | 540±180 | 0.314 | ||
| Amplitude (mV) | Average | 20±10 | 20±10 | 20±10 | 0.519 | |
| Peak | 60±30 | 60±30 | 70±30 | 0.399 | ||
| MHAM | Time (ms) | Onset | −290±110 | −300±100 | −290±100 | 0.751 |
| Offset | 210±70 | 190±70 | 190±80 | 0.489 | ||
| Duration | 490±150 | 490±120 | 480±160 | 0.741 | ||
| Amplitude (mV) | Average | 30±30 | 20±10 | 30±10 | 0.325 | |
| Peak | 80±30 | 80±40 | 90±40 | 0.116 | ||
| LHAM | Time (ms) | Onset | −250±70 | −290±70 | −280±70 | 0.135 |
| Offset | 240±100 | 220±110 | 210±120 | 0.344 | ||
| Duration | 490±130 | 500±130 | 480±120 | 0.740 | ||
| Amplitude (mV) | Average | 40±40 | 30±10 | 30±10 | 0.355 | |
| Peak | 100±50 | 100±50 | 90±40 | 0.905 | ||
| MGAS | Time (ms) | Onset | 20±80 | 20±80 | 40±10 | 0.681 |
| Offset | 590±70 | 620±70 | 600±80 | 0.110 | ||
| Duration | 560±120 | 610±130 | 560±140 | 0.133 | ||
| Amplitude (mV) | Average | 40±10 | 40±30 | 40±20 | 0.818 | |
| Peak | 110±40 | 100±40 | 120±60 | 0.101 | ||
| LGAS | Time (ms) | Onset | 70±160 | 70±170 | 60±150 | 0.889 |
| Offset | 560±70 | 610±60‡,Δ | 580±80 | 0.004* | ||
| Duration | 480±160 | 520±190 | 500±210 | 0.584 | ||
| Amplitude (mV) | Average | 40±20 | 30±20‡ | 40±20 | 0.037* | |
| Peak | 110±40 | 100±60 | 110±70 | 0.624 | ||
| TA | Time (ms) | Onset | −410±180 | −420±170 | −450±160 | 0.428 |
| Offset | 240±180 | 230±140 | 230±130 | 0.856 | ||
| Duration | 650±180 | 650±170 | 690±100 | 0.548 | ||
| Amplitude (mV) | Average | 50±20 | 50±30 | 50±30 | 0.662 | |
| Peak | 150±50 | 170±120 | 160±90 | 0.435 | ||
Abbreviations as follows: ms, millisecond; mV, millivolt; GMAX, gluteus maximus; GMED, gluteus medius; RF, rectus femoris; VM, vastus medialis; VL, vastus lateralis; MHAM, medial hamstring; LHAM, lateral hamstring; MGAS, medial gastrocnemius; LGAS, lateral gastrocnemius; and TA, tibialis anterior. Data are presented as mean±standard deviation. Negative and positive times are pre- and post-heel strike, respectively.
Relative to no brace, the adjusted brace reduced average amplitude of GMAX (−4mV [−6, −1], p=0.015) and LGAS (−9mV [−16, −2], p=0.020). There were no other statistically significant differences observed between the three test conditions (Table 1).
DiscussionIn younger adults with predominant lateral knee OA and valgus malalignment after ACLR, an unloader brace did not significantly change co-contraction of agonist and antagonist muscles in the lower limb but produced changes in the timing of GMAX, GMED and LGAS, and amplitude of GMAX and LGAS.
Ramsey et al.15 proposed that reductions in knee pain reported by individuals with medial OA when wearing a valgus unloader knee brace could be due to reduced muscle co-contraction and subsequent reduction of joint loading, rather than mechanical unloading from an opposing valgus force. Fantini Pagani et al.27 also reported significant decreases in muscle group (flexor-extensor) and pair (VL/LHAM and VM/MHAM) co-contraction patterns when individuals with medial knee OA walked with a valgus brace. However, we observed no significant differences in muscle co-contraction patterns during walking in individuals with lateral knee OA after ACLR with a varus unloader brace, despite the significant differences in knee angles and moments that we observed with a varus unloader brace.13 An unloader brace can improve knee pain, stability and confidence during high-demand activities in individuals with knee OA after ACLR.12 These results indicate that improvements in knee symptoms are likely not related to muscle co-contraction.
The majority of muscle activation changes that we observed with the knee brace occurred proximally. Relative to no brace, the brace significantly delayed offset (37%), and reduced average activation amplitude (16%) of GMAX and resulted in earlier onset of GMED (31%). Interestingly, the only knee spanning muscle to demonstrate an immediate change in activation with the knee brace was LGAS, with the brace resulting in delayed offset (8%) and reduced average activation amplitude (25%). To our knowledge, there are no studies that have compared muscle activity in individuals with post-traumatic lateral knee OA or non-traumatic lateral knee OA, and it would not be appropriate to compare the results of the current study with previous literature, as most knee OA studies have either excluded cases with lateral knee OA or pooled them with medial knee OA. Thus, the clinical relevance of these changes is not clear.
The addition of mechanical correction by the brace — to correct for the valgus malalignment — mostly did not influence the EMG of lower limb muscles. These findings appear to align with our previous research,13 which revealed no significant mechanical differences between adjusted and unadjusted brace conditions in individuals with lateral knee OA after ACLR during walking. Combined, these findings suggest the brace, regardless of varus realignment, can produce significant changes in biomechanics,13 and affect activation patterns of GMAX and LGAS in individuals with predominant lateral knee OA after ACLR. Further research is needed to determine the effects of varus unloader brace on contact forces in this patient-population.
A number of limitations of this study should be acknowledged. First, due to sample size, we were unable to explore the effects of factors such as radiographic severity and sex on the bracing response. Second, we did not compare our lateral knee OA after ACLR data with healthy controls. Thus, further research is required to determine whether individuals with lateral knee OA after ACLR have altered lower-limb muscle activation patterns compared to healthy controls or individuals with non-traumatic lateral knee OA. Third, due to the within-subject nature of the study, it was not possible to blind participants to the brace. Thus, the changes observed could have been partially due to placebo effects.
ConclusionsIn younger individuals with lateral knee OA after ACLR, the unloader knee brace did not change muscle co-contraction; however, changes in GMAX, GMED, and LGAS timing and amplitude parameters were observed. The improvements in knee symptoms previously reported in individuals with knee OA after ACLR with an unloader brace are likely not mediated by altered muscle co-contraction patterns.
Authors’ contributionsAll authors were fully involved in drafting the article and all authors approved the final version to be submitted for publication. The authors’ contributions are as follows: conception and design: Hart, Collins, Crossley; data acquisition: Hart, Collins; data processing and analysis: Hart, Holt, Semciw, Crossley; data interpretation: Hart, Semciw, Collins, Crossley; and drafting the article: Hart, Holt, Semciw, Collins, Crossley.
Conflicts of interestThe authors declare no conflicts of interest.
DJO Global provided knee braces and funding for the radiographs. The study sponsors had no involvement in the study design, in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.