Incentive spirometers (ISs) are clinical devices used in respiratory physical therapy to increase alveolar ventilation and functional residual capacity.
ObjectivesTo investigate factors that influence physical therapists from Minas Gerais in selecting a type of IS and the scientific background behind the use of ISs by physical therapists who work with patients with respiratory dysfunctions.
MethodsPhysical therapists from 13 hospital and non-hospital institutions (public/private) completed a self-administered questionnaire based on the current evidence on ISs.
ResultsIndications and contraindications of ISs are not fully understood by most of the 168 physical therapists who completed the questionnaire. Volume-oriented IS was preferred over flow-oriented IS. However, only half of the physical therapists have a scientific background to justify the choice of one IS type rather than the other.
ConclusionsMost physical therapists from Minas Gerais do not fully understand the indications and contraindications for ISs. Despite physical therapists stating their preference for volume-oriented IS, this choice is not necessarily based on current scientific evidence. The development of strategies to bring physical therapists closer to evidence-based practice is necessary to ensure best patient care.
An incentive spirometer (IS) is a device that stimulates the achievement of maximum sustained inspirations through visual and/or auditory feedback.1-3 It is widely used in clinical practice to increase alveolar ventilation and functional residual capacity in conditions in which lung ventilation is impaired or at risk.1,4,5 According to the parameters to be reached, the IS can be classified as flow-oriented IS or volume-oriented IS,1,6 promoting distinct ventilatory responses.7-9
The superiority of volume-oriented IS over flow-oriented IS has been previously demonstrated, with a higher inspiratory time,7,9-12 a lower respiratory rate,8,9 and a lower recruitment of accessory muscles.9,11-14 Therefore, volume-oriented IS provides a more laminar airflow during inspiration, which results in a more uniform alveolar ventilation, being more effective in promoting the targeted physiological effects.8-11
To achieve the desired patient outcomes it is necessary to understand the concepts of evidence-based practice and to apply them on the delivery of health care. Therefore, the best practice involves research-based knowledge and its implementation on treatment. Considering the superiority of volume-oriented IS over flow-oriented IS and the main objective of this device, it is important to investigate the physical therapists knowledge to assure the delivery of best care.
In this context, this study aimed to investigate the aspects of clinical practice that influence professionals to select an IS type and the scientific background behind the use of ISs by physical therapists from Minas Gerais who work with patients with respiratory dysfunctions.
MethodsStudy design and participantsThis was a cross-sectional study. Physical therapists from Belo Horizonte, Minas Gerais, Brazil, who work with patients with respiratory dysfunction regardless of age, sex, race, socioeconomic status, year of graduation, and professional degree were recruited. Exclusion criteria were: the inability to understand the questionnaire or refusal to participate in the study. All participants gave written informed consent and their rights were protected. The study was approved by the Ethics Committee of the Universidade Federal de Minas Gerais, Brazil (CAAE: 65200717.7.0000.5149).
Measuring toolA self-administered questionnaire of 14 multiple-choice questions was developed by three professionals who had clinical and research experience in the respiratory physical therapy field. The questionnaire was used as a tool to outline the knowledge of physical therapists working with patients with respiratory dysfunctions in Minas Gerais. Furthermore, socio-demographic data (age, working hours, year of graduation, professional degree, length of professional experience with patients with respiratory dysfunction, and characteristics of the working institutions) were also collected to better describe this study's sample. The questionnaire also included questions about the use of scientific literature in English and the frequency of access to scientific databases.
The questionnaire addressed topics already well established in the scientific literature regarding ISs. Questions regarding clinical practice concepts such as aims, indications, contraindications, and instructions provided to patients for the use of ISs were based on the last clinical practice guideline for IS use1 and on the paper by Armstrong.3 For the contraindications, we have also used the study of Goldstein et al.15 to support the questionnaire's alternatives on IS use by patients with tracheostomy. Questions regarding the rationale behind the superiority of volume-oriented IS when compared to flow-oriented IS were based on the latest studies of Paisani et al.,11 Lunardi et al.,12 and Parreira et al.10
ProceduresData collection took place in 13 hospital and non-hospital institutions (public and private). The aims and procedures of this study were clarified to the managers of the services who were asked to encourage physical therapists to participate in the study. It was agreed that the feedback on results would be provided through scientific publications as aggregate data and not individually, as this study aimed to provide a broad overview of the knowledge of physical therapists working with patients with respiratory dysfunctions.
The initial contact with the physical therapists was made by telephone or e-mail, with the subsequent distribution and collection of questionnaires made in person. Participants were instructed not to leave questions unanswered and to respond to the questionnaires individually and without consultations. They were also instructed to choose only one alternative for each question, except for one of the questions, in which they were informed that more than one answer would be accepted.
The researchers distributed and recollected the self-administered questionnaires from the participants using opaque and sealed envelopes to maintain the confidentiality of the responses and the anonymity of the participants.
Sample sizeThe sample was non-probabilistic and based on the percentage of registered professionals and/or specialists in respiratory physical therapy in Minas Gerais, obtained via the Brazilian Association of Cardiorespiratory Physiotherapy and Physiotherapy in Critical Care (ASSOBRAFIR), which supported this study. A finite population of 210 physical therapists was estimated for the state of Minas Gerais with an assumed proportion of 50% in Belo Horizonte. The calculation determined a sample size of 137 physical therapists based on a margin of error of 5%. The proportion of 50% was adopted because the distribution of physical therapists in the state of Minas Gerais was unknown and this was a conservative approach.16
Data analysisDescriptive statistics were presented as measure of central tendency (mean), variability (standard deviation), and frequencies. The normality of data distribution was verified by the Shapiro-Wilk test. Comparisons between professionals from public versus private institutions were performed using the difference of two independent samples proportions test. To evaluate bivariate associations between participant characteristics (age, time of professional experience, workplace, higher professional degree, and use of scientific literature in English) and the number of errors on the questionnaire, the Spearman correlation coefficient was used. The strength of the correlations was defined as ≥ 0.30 to 0.49 as weak, ≥ 0.50 to 0.69 as moderate, ≥ 0.70 as strong, and 1.0 as perfect.17 The variables included in the model of multiple linear regression were selected from the correlation analyses. The variables that presented correlation to the number of errors on the questionnaire and that were not highly correlated with each other were tested in the model. The criteria for inclusion were based on p value < 0.10.18 In the final model, only the variables that were statistically significant remained. The level of significance adopted was p < 0.05. The multiple linear regression was designed using the stepwise method. The final model was determined by the adjusted coefficient of determination (R2) and by the statistical significance. To determine the statistical quality of the model, the absence of multicollinearity was verified by the variance inflation factor (VIF>5.0) and normal distribution of residuals by Shapiro-Wilk test and graphic visual analysis (Q-Q plot). The Statistical Package for the Social Sciences v 15.0 (Chicago, IL, USA) and Minitab v. 16 (State College, PA, USA) were used for analyzes.
ResultsParticipant characteristicsTwo hundred and forty-seven physical therapists were recruited and received a printed copy of the questionnaire. From these, 168 (68%) completed the questionnaires and 79 (32%) refused to participate. Seventy-eight (46%) physical therapists were from public institutions while 90 (54%) were from private institutions. The age of the participants ranged from 23 to 56 years with a mean of 34.0 ± 7.6 years. The duration of professional experience working with patients with respiratory dysfunctions ranged from 1 to 33 years, with a mean of 9.0 ± 7.2 years. Most of the physical therapists worked in hospitals (88.1%), fulfilled a workload of 30 hours per week (70.2%), and had a postgraduate degree as their higher professional degree (84.5%). The proportion of physical therapists with a postgraduate degree in public and private institutions was 94% and 77%, respectively.
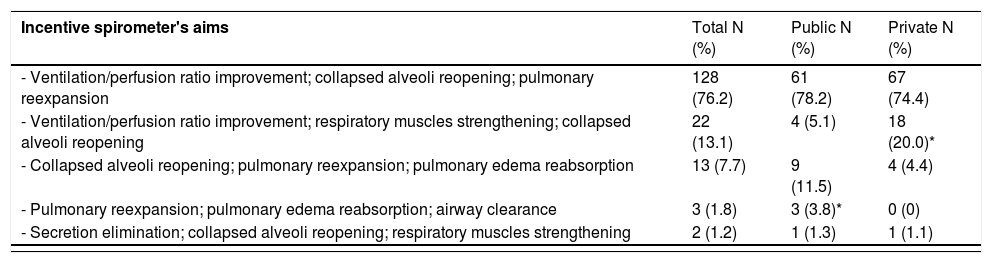
Aspects of clinical practiceTable 1 shows the absolute number and frequency of answers concerning IS concepts addressed by the questionnaire. Participants were also divided into two sub-groups according to the institution they work for (public or private). Most professionals understand the aims of these devices and correctly instruct patients on their use for both types of IS, however, they do not seem to know the main indications and contraindications for IS.
Distribution of the responses regarding clinical practice concepts.
| Incentive spirometer's aims | Total N (%) | Public N (%) | Private N (%) |
|---|---|---|---|
| - Ventilation/perfusion ratio improvement; collapsed alveoli reopening; pulmonary reexpansion | 128 (76.2) | 61 (78.2) | 67 (74.4) |
| - Ventilation/perfusion ratio improvement; respiratory muscles strengthening; collapsed alveoli reopening | 22 (13.1) | 4 (5.1) | 18 (20.0)* |
| - Collapsed alveoli reopening; pulmonary reexpansion; pulmonary edema reabsorption | 13 (7.7) | 9 (11.5) | 4 (4.4) |
| - Pulmonary reexpansion; pulmonary edema reabsorption; airway clearance | 3 (1.8) | 3 (3.8)* | 0 (0) |
| - Secretion elimination; collapsed alveoli reopening; respiratory muscles strengthening | 2 (1.2) | 1 (1.3) | 1 (1.1) |
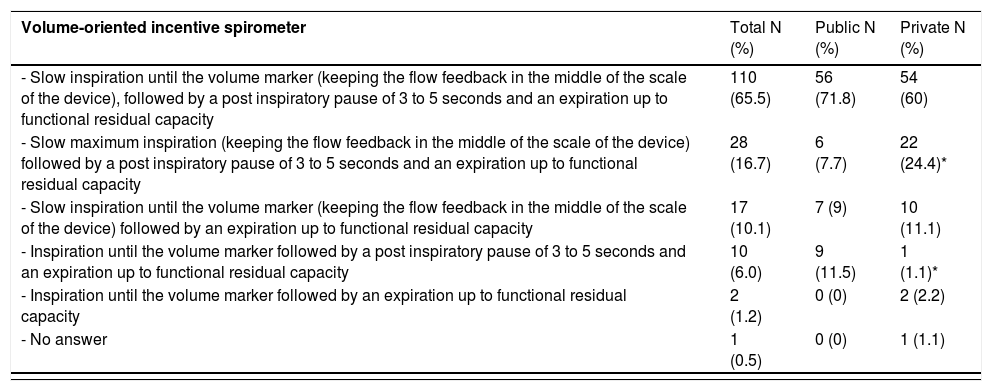
Table 2 shows the instructions provided to patients for ISs use for the total group and for physical therapists from public and private institutions (absolute number and frequency). Half of the sample prescribes the targeted tidal volume in volume-oriented IS according to 5-8 mL/kg predicted body weight.
Distribution of the responses regarding the instructions provided to patients for the use of the incentive spirometer.
| Volume-oriented incentive spirometer | Total N (%) | Public N (%) | Private N (%) |
|---|---|---|---|
| - Slow inspiration until the volume marker (keeping the flow feedback in the middle of the scale of the device), followed by a post inspiratory pause of 3 to 5 seconds and an expiration up to functional residual capacity | 110 (65.5) | 56 (71.8) | 54 (60) |
| - Slow maximum inspiration (keeping the flow feedback in the middle of the scale of the device) followed by a post inspiratory pause of 3 to 5 seconds and an expiration up to functional residual capacity | 28 (16.7) | 6 (7.7) | 22 (24.4)* |
| - Slow inspiration until the volume marker (keeping the flow feedback in the middle of the scale of the device) followed by an expiration up to functional residual capacity | 17 (10.1) | 7 (9) | 10 (11.1) |
| - Inspiration until the volume marker followed by a post inspiratory pause of 3 to 5 seconds and an expiration up to functional residual capacity | 10 (6.0) | 9 (11.5) | 1 (1.1)* |
| - Inspiration until the volume marker followed by an expiration up to functional residual capacity | 2 (1.2) | 0 (0) | 2 (2.2) |
| - No answer | 1 (0.5) | 0 (0) | 1 (1.1) |
| Flow-oriented incentive spirometer | |||
|---|---|---|---|
| - Slow deep inspiration with elevation of 1 sphere, followed by a post inspiratory pause of 3 to 5 seconds and an expiration up to functional residual capacity | 91 (54.2) | 50 (64.1)* | 41 (45.6) |
| - Slow deep inspiration with elevation of all the spheres, followed by a maximum post inspiratory pause and an expiration up to functional residual capacity | 31 (18.5) | 12 (15.4) | 19 (21.1) |
| - Vigorous inspiration with elevation of as many spheres as possible, followed by a post inspiratory pause of 3 to 5 seconds and a forced expiration up to functional residual capacity | 22 (13.1)18 (10.7) | 10 (12.8)4 (5.1) | 12 (13.3)14 (15.6)* |
| -Slow deep inspiration with elevation of 1 sphere and an expiration up to functional residual capacity | |||
| - Quick strong inspiration with elevation of 2 spheres, followed by a post inspiratory pause of 3 to 5 seconds and an expiration up to functional residual capacity | 3 (1.8) | 1 (1.3) | 2 (2.2) |
| - No answer | 3 (1.7) | 1 (1.3) | 2 (2.2) |
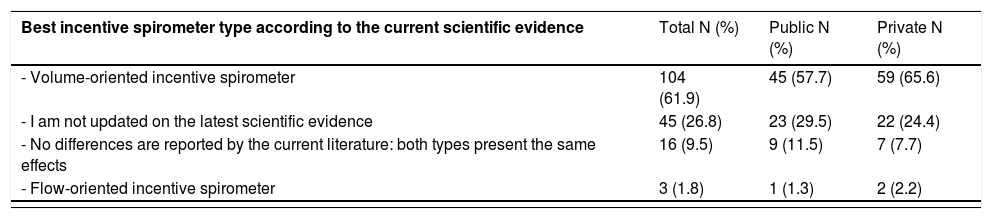
Table 3 presents information about the use of evidence-based practice. Most physical therapists are aware that the current scientific evidence indicates a superiority of volume-oriented IS compared to flow-oriented IS. A moderate percentage of professionals were aware of the different physiological effects described in the literature for both types of IS. The majority of professionals access scientific databases only when necessary and always in English. Most physical therapists who did not use scientific literature in English worked in private institutions.
Distribution of the responses regarding the evidence-based practice.
| Update on the scientific evidence on the physiological effects of incentive spirometer types | |||
|---|---|---|---|
| - Volume-oriented incentive spirometer recruits less accessory muscles than flow-oriented incentive spirometer and flow-oriented incentive spirometer promotes higher respiratory rates than volume-oriented incentive spirometer | 85 (50.6) | 43 (55.1) | 42 (46.7) |
| - The physiological effects of both incentive spirometer types are the same, the only difference is the feedback mechanism of the devices | 47 (28.0) | 22 (28.2) | 25 (27.8) |
| - Flow-oriented incentive spirometer promotes a higher inspiratory time than volume-oriented incentive spirometer and volume-oriented incentive spirometer recruits less accessory muscles than flow-oriented incentive spirometer | 16 (9.5) | 2 (2.6) | 14 (15.6)* |
| - Volume-oriented incentive spirometer generates a higher respiratory workload than flow-oriented incentive spirometer and flow-oriented incentive spirometer promotes a higher inspiratory time than volume-oriented incentive spirometer | 9 (5.4) | 4 (5.1) | 5 (5.5) |
| - Flow-oriented incentive spirometer promotes a better pulmonary reexpansion than volume-oriented incentive spirometer and flow-oriented incentive spirometer promotes higher respiratory rates than volume-oriented incentive spirometer | 6 (3.6) | 5 (6.4)* | 1 (1.1) |
| - No answer | 5 (2.9) | 2 (2.6) | 3 (3.3) |
| Frequency of access to scientific databases | |||
|---|---|---|---|
| - Only when I need to do it | 74 (44.0) | 40 (51.3)* | 34 (37.8) |
| - Once a week or more | 39 (23.2) | 9 (11.5) | 30 (33.3)* |
| - Once a month | 34 (20.2) | 17 (21.8) | 17 (18.9) |
| - Every 3 months | 15 (8.9) | 9 (11.5) | 6 (6.6) |
| - Every 6 months | 2 (1.2) | 0 (0) | 2 (2.2) |
| - I never do it | 2 (1.2) | 2 (2.6) | 0 (0) |
| - Every year | 1 (0.6) | 1 (1.3) | 0 (0) |
| - No answer | 1 (0.7) | 0 (0) | 1 (1.1) |
The sources to access information ranged from books, scientific articles, co-workers’ experience, courses, and scientific events. Twenty-nine percent of the professionals reported the use of all these options and 13.7% prioritizes the use of scientific articles as the source of information.
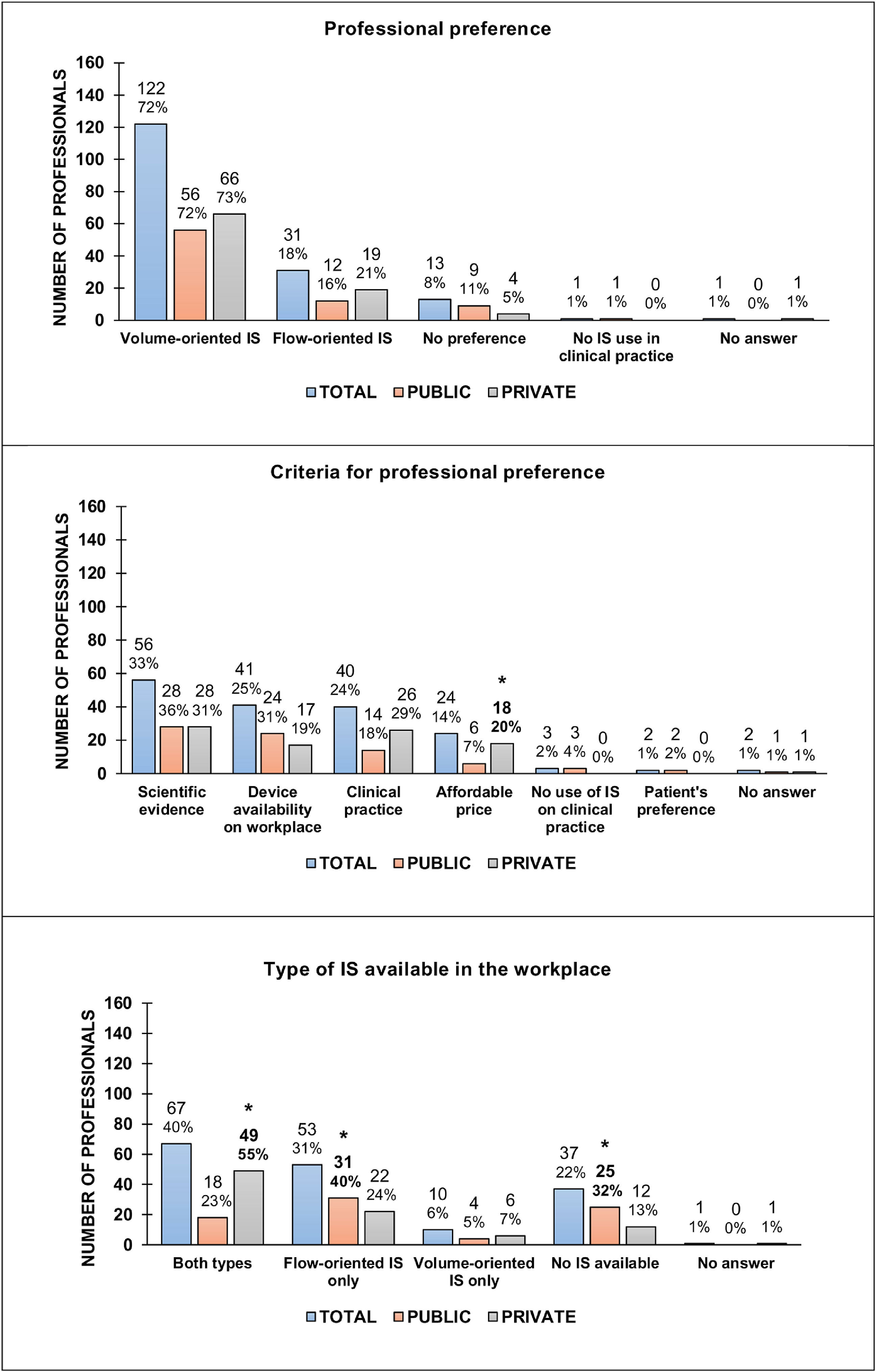
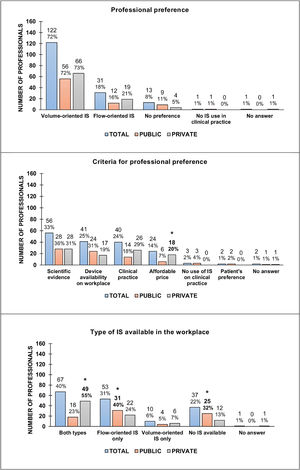
Choice of the IS typeFigure 1 presents the aspects related to the choice of an IS type for the total group and for physical therapists from public and private institutions. Most of the physical therapists preferred volume-oriented IS and the main reasons to justify this choice were “scientific evidence,” “equipment available in my workplace,” and “my clinical practice.” Twenty-two percent (37/168) of the physical therapists do not have access to both types of IS in their workplaces, and flow-oriented IS is usually the most available spirometer (53/168). Both IS types are usually found in private hospital and non-hospital institutions, while in a public setting, either for hospital and non-hospital institutions, flow-oriented IS was the most available spirometer.
Aspects that influence the selection of an incentive spirometer type. Data were presented in absolute numbers and percentages. IS, incentive spirometers; *, p<0.05 (comparisons between Public and Private institutions). The total number of respondents was 168; 78 from the public sector and 90 from the private sector. Percentages were rounded to clear the illustration.
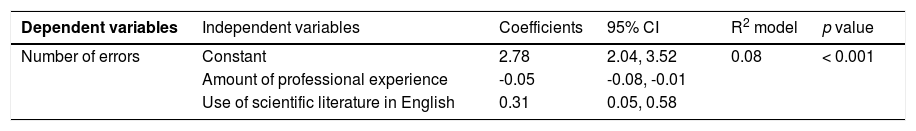
The variables age (rho = -0.15, p = 0.049), length of professional experience (rho = -0.24, p = 0.002), workplace (rho = -0.16, p = 0.04), higher professional degree (rho = -0.17, p = 0.03), and use of scientific literature in English (rho = 0.22, p = 0.005) were associated with the number of errors on the questionnaire (Table 4). The length of professional experience and the use of scientific literature in English are the factors, which potentially reduce the number of errors on the questionnaire (R2 = 0.08, p < 0.001).
Model obtained by regression analysis for the influence of variables on the number of errors on the questionnaire.
| Dependent variables | Independent variables | Coefficients | 95% CI | R2 model | p value |
|---|---|---|---|---|---|
| Number of errors | Constant | 2.78 | 2.04, 3.52 | 0.08 | < 0.001 |
| Amount of professional experience | -0.05 | -0.08, -0.01 | |||
| Use of scientific literature in English | 0.31 | 0.05, 0.58 |
CI, confidence intervals for coefficients; R2, coefficient of determination.
The main results of this study were: 1) Gaps concerning the knowledge of the ISs indications and contraindications were identified for most of the physical therapists who work with patients with respiratory dysfunctions; 2) Volume-oriented IS was preferred by most of the professionals, however, only half of the sample has a scientific background to justify the choice of an IS type over the other; 3) Flow-oriented IS was the most available type in public institutions.
The ISs are therapeutic devices indicated for the improvement of alveolar ventilation and functional residual capacity in conditions of reduced lung compliance.1 Despite the wide use of IS in pre and post-operative care of individuals with thoracic and upper abdominal surgeries,1 and its documented benefits in decreasing respiratory rate, increasing tidal volume,8 and improving pulmonary function,14 less than half of the physical therapists evaluated in this study knew IS indications. In addition, 10% of them considered the IS as a device indicated to promote respiratory muscles strengthening. It is true that IS has been used for respiratory muscle training,19,20 however, other devices such as Threshold® and PowerBreathe® have been developed specifically for this purpose.21
The majority of the physical therapists considered the IS contraindicated for patients with tracheostomy, which is not true and completely possible if an adapter is used.16 In contrast, the use of IS is contraindicated for nonresponsive individuals, such as people in coma or presenting difficulty to understand the necessary instructions to correctly perform the exercise (e.g. children smaller than four years old).1
Most of the participants were aware of the superiority of the volume-oriented IS compared to flow-oriented IS, however, only half of the sample knew the differences between the physiological effects of both types of IS reported by the literature. Previous studies indicate that volume-oriented IS promotes a greater increase of the inspiratory time8-12 and a greater decrease of the respiratory rate compared to flow-oriented IS.8,9 In addition, electromyographic findings show that flow-oriented IS recruits more accessory musculature during inspiration,9,22 Therefore, although both types of IS are indicated for pulmonary reexpansion, the physiological effects of the volume-oriented IS on ventilation are more consistent with the aims of this device. Recently, Eltorai et al.23 showed the discrepancy between health care professionals’ beliefs and the evidence data supporting IS use. The authors highlighted that schools or clinical training at workplaces might be an opportunity to integrate evidence-based care into future practice.
Different instructions for the target volume in volume-oriented IS are found in the literature, such as maximal inspirations;8,9,22 slow deep inspirations;24 deep inspirations sustained for 5 to 10 seconds;14,25 slow deep inspirations sustained for 3 seconds;6,26 or for 5 seconds.11,12,27 In the present study, we observed that most of the physical therapists use the calculation of the ideal weight multiplied by 5-8 mL/kg as a volume prescription for the volume-oriented IS. The preference for this prescription is probably associated with the recommendation for protective ventilation of mechanically ventilated patients.28
Different instructions were also found in the literature for the use of the flow-oriented IS: slow deep inspirations;24 slow deep inspirations sustained for 3 seconds6,26 and for 5 seconds;11,12,14,27 inspiration with elevation of the three spheres for as long as possible23 and inspiration with elevation of two spheres.9,10 In this study, the instruction to raise only the first sphere of the device was considered as the correct answer by more than half of the physical therapists, based on the concept that this strategy provides a less turbulent inspiratory flow and recruits less accessory musculature. A recent update on why, how, and when to use the IS considers a slow and maximum inspiration followed by an inspiratory pause of 3 to 5 seconds as a mandatory instruction before the use of both types of IS.3
This study did not aim to address the effectiveness of the IS through the questionnaire. We have used the questionnaire as a tool to get a picture of the knowledge of physical therapists working with patients with lung dysfunctions regarding topics already well established in the scientific literature, such as the aims, indications, contraindications, and known physiological effects of the IS and the main differences between volume and flow-oriented devices.1,3,10-12 In addition, we believe that the lack of evidence on IS effectiveness might be associated with gaps in the knowledge regarding its use in clinical practice. Our findings showed that most professionals do not fully understand the correct indications and contraindications of the IS. Therefore, improving professional's awareness about the current scientific evidences and the rationale behind ISs use is a necessary step to lead up to the development of new studies elucidating the role of this resource in clinical practice.
Almost 85% of the physical therapists of our sample were specialists, masters of science, or doctors in philosophy, which, in theory, makes these professionals more qualified for clinical practice. Our results have shown that the length of professional experience and the lack of use of scientific literature in English were the main aspects related to errors in the questionnaire. Therefore, professionals should find strategies to improve reading skills in English to keep up-to-date with the best scientific evidence.
There was an increase in the difference between private and public healthcare settings in the 1990s after the implementation of the Brazilian Unified Health System.29 Our results highlight this contrast regarding the availability of the ISs. The lower availability of volume-oriented IS in public institutions is probably due to its four times higher price when compared to the flow-oriented IS.10
This study sent questionnaires only to physical therapists working in the city of Belo Horizonte. Thus, the results may not be representative of the entire population of physical therapists if we consider a national spectrum. Further investigation in other regions of the country would provide a broader national portrait, contributing to the external validity of the data.
ConclusionsMost of the physical therapists from Minas Gerais who work with patients with respiratory dysfunctions do not fully understand the correct indications and contraindications of ISs. Physical therapists stated their preference for volume-oriented IS, however, this choice is not necessarily based on the current scientific evidence, because many professionals were not aware of the physiological effects that justify the superiority of the volume-oriented IS compared to flow-oriented IS. The development of strategies to bring the physical therapists closer to evidence-based practice is a necessary action to guarantee the best care for patients with respiratory dysfunctions.
We are grateful to all the physical therapists who have participated in this study. We also would like to thank the Brazilian Association of Cardiorespiratory Physiotherapy and Physiotherapy in Critical Care (ASSOBRAFIR) for the support with information that helped us to calculate a representative sample of professionals from the city in which this study was conducted. The work was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Finance Code 001 and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Grant 309990/2017-3. The funding sources had no role in the design, conduct, or reporting of this study.