A better understanding about the relationship between trunk and hip muscles strength and core stability may improve evaluation and interventions proposed to improve core stability.
ObjectivesTo investigate if trunk and hip muscles strength predict pelvic posterior rotation during the bridge test with unilateral knee extension.
MethodsThis is a cross-sectional study. Sixty-one healthy individuals of both sexes (age, 28±6.4 years, weight, 66.5±10.9kg, height, 167±9.5cm) performed the bridge test with unilateral knee extension. The pelvic posterior rotation during the bridge test was obtained with two-dimensional video analysis. Isometric strength of the trunk extensors and rotators, and hip abductors, external and internal rotators and extensors were measured with a hand-held dynamometer. Multiple linear regression analysis was performed to identify if the strength variables could explain the pelvic posterior rotation during the test.
ResultsMuscle strength predicted pelvic posterior rotation during the bridge test (r=0.54; p=0.003). Strength of the trunk rotators (p=0.045) and hip internal rotators (p=0.015) predicted reduced magnitude of pelvic posterior rotation during the bridge test, and strength of the hip extensors (p=0.003) predicted increased magnitude of pelvic posterior rotation.
ConclusionsTrunk rotators and hip internal rotators and extensors strength predict 29% of the performance during the bridge test with unilateral knee extension. The strength of these muscles should be evaluated in individuals with increased pelvic posterior rotation during the bridge test with unilateral knee extension.
Core stability can be defined as the capacity to control the position and movement of the trunk relative to the pelvis to allow energy production, transference and absorption from the distal and proximal segments during the performance of different tasks.1,2 The core complex consists of different groups of muscles (e.g. abdominals, paraspinal and hip muscles).3 In theory, some factors, such as neuromuscular control and the capacity of the core muscles to generate tension, can influence core stability. Therefore, core muscles weakness may compromise core stability and consequently worsen performance,4 affect motion pattern during different tasks5 and contribute to the development of injuries.6
The relationship between core stability, trunk and hip muscles strength is not clear.6–9 Barbado et al.9 demonstrated weak correlations between trunk extensors strength and the anterior and posterior trunk angular displacement in a seated position after sudden loading in athletes. In a different study with athletes, Leetun et al.6 also demonstrated weak correlations between hip strength and the total time spent in the side bridge position. Previous studies focused on the relationship between trunk flexors and extensors strength and core stability8,9 in spite of the fact that core stability involves other muscles and the capacity to control movement in the three planes of motion. In this sense, trunk rotators strength may be as important as trunk flexors and extensors strength to core stability. In addition, although trunk and hip muscles strength may collectively influence core stability, previous studies have only investigated pairwise correlations between individual muscles strength and core stability and focused on either trunk or hip muscles strength,6–9 which might have hampered demonstrating this relationship. Therefore, although reduced core stability is commonly associated with reduced trunk and hip muscles strength in clinical settings, this assumption is not currently supported by scientific evidence.
There are different clinical tests to evaluate core stability, such as the side and prone bridge tests.2,10–14 However, the performance in some of these tests is measured by the time the individual is able to spend in a bridge test position. Therefore, upper limbs and distal lower limbs muscles may counterbalance poor performance of the core muscles2 and consequently increase time in the test position. The bridge test with unilateral knee extension is an alternative to reduce the influence of upper arms and distal lower limbs muscles, since performance during this test is determined exclusively by the individual's ability to maintain pelvic alignment.10 In fact, a recent study demonstrated that, unlike a trunk endurance test,2 the bridge test with unilateral knee extension is a valid clinical test to measure core stability.2 The purpose of this study was to investigate if trunk and hip muscles strength predict pelvic posterior rotation during the bridge test with unilateral knee extension in healthy individuals. We hypothesized that the strength of the trunk and hip muscles would predict reduced magnitude of pelvic posterior rotation during the bridge test with unilateral knee extension.
Materials and methodsSubjectsThe sample size was defined based on the criterion of 10 participants for each independent variable in the regression model, which resulted in a minimum sample size of 60 participants. Seventy healthy adults of both sexes were recruited by convenience for this study. The inclusion criteria were (i) age between 18 and 45 years old, (ii) no history of pain, injuries or surgeries on the lower limbs and trunk in the past six months and (iii) not having neurologic, cardiorespiratory, rheumatologic or chronic orthopedic health conditions. These criteria were self-reported and assessed by a trained and experienced physical therapist. The exclusion criteria were (i) report of discomfort or pain during data collection, and (ii) inability to perform the procedures of data collection. Nine participants were excluded for not being able to extend the hip of support during the bridge test. Therefore, 61 individuals were included in this study. Each participant signed a written consent form approved by the Ethical Research Committee of the Universidade Federal dos Vales do Jequitinhonha e Mucuri, Belo Horizonte, Minas Gerais, Brazil (CAEE 51620715.9.0000.5108).
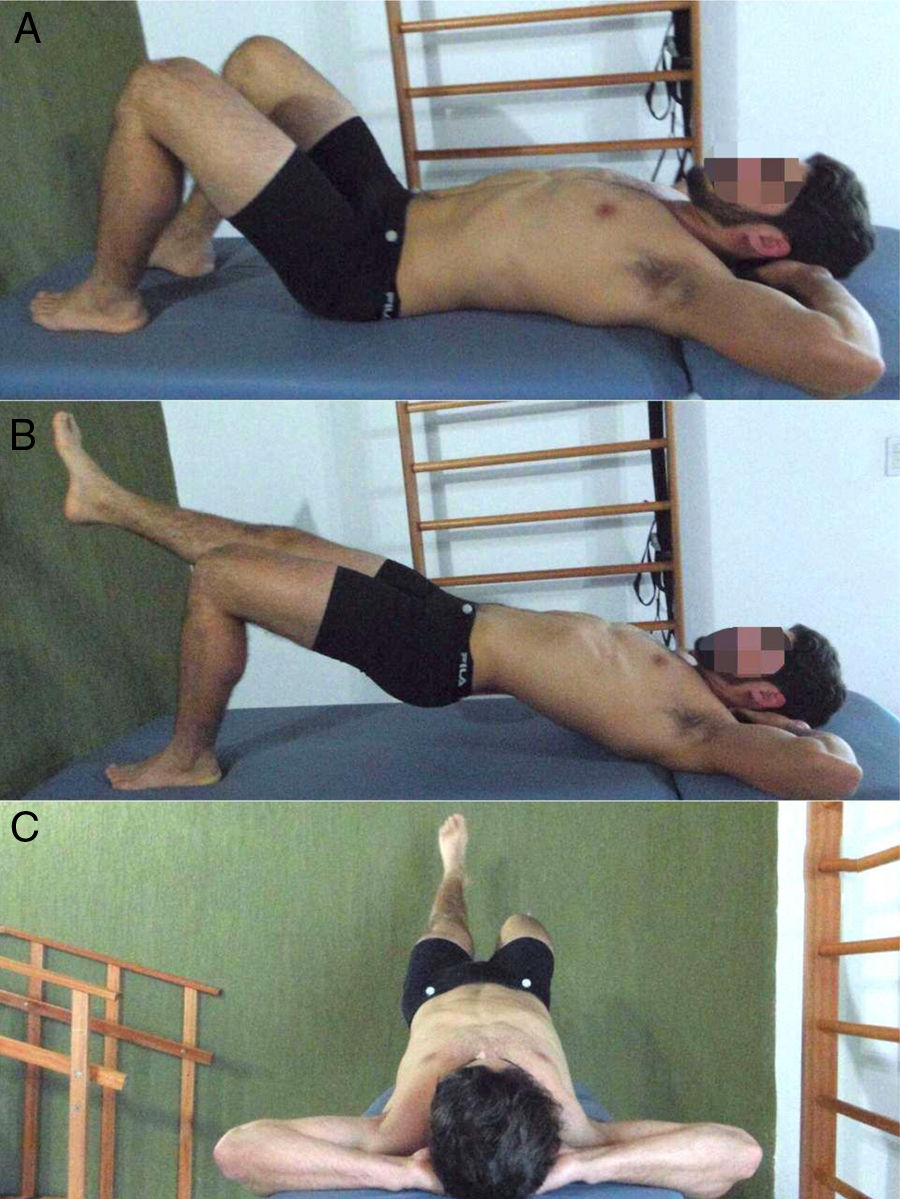
ProceduresThe participants were instructed not to perform physical exercises at least 24h prior to data collection. Initially, the participants answered the International Physical Activity Questionnaire (IPAQ).15 Lower limb dominance was defined based on the participants’ answer to the following question: what leg would you use to kick a ball as far as possible16? Following this, the participant performed the bridge test with unilateral knee extension. The bridge test with unilateral knee extension was performed following the methods of a previous study.10 A trained examiner positioned reflective markers on the participant's anterior superior iliac spines. Then, the participant laid down on the treatment table in supine position, with hands positioned under the head, hips and knees flexed in a self-selected range of motion and with the feet supported on the treatment table. The self-selected knee flexion was used to guarantee that participants were comfortable during testing and that the position selected was the most adequate to each participant's anthropometrics characteristics.10 Participants were instructed to raise their pelvis and perform unilateral knee extension of the dominant lower limb, maintaining the elevated thigh (i.e. dominant thigh) at the same level as the thigh of the support side (i.e. non-dominant side) (Fig. 1). In addition, the participant was instructed to maintain the trunk, pelvis and dominant lower limb on a straight line during the test. This position was sustained during 10s and the test was repeated three times. The participants rested for 60s between repetitions. The participant performed one trial of familiarization before starting data collection. The examiner used the same instructions for all of the participants. The test was interrupted and repeated if the examiner perceived compensations such as pelvic retroversion and hip flexion and abduction on the support limb.
The pelvic posterior rotation during the test was measured following the methods proposed by Andrade et al.10 The examiner registered the bridge test with a digital camera (DSC-HX1, Sony, 9.1 Mpixel, CMOS HD) positioned on a tripod 80cm distant from the extremity of the treatment table. The camera was parallel to the ground, which was assured by means of an inclinometer (Mundo Sat, Brazil). The height of the camera was adjusted for each participant, which allowed the plane of the camera for image capture to be orthogonal to the pelvic transverse plane during the test. In addition, the pelvis was centralized in the camera view. To quantify the magnitude of pelvic posterior rotation during the bridge test, we performed a two-dimensional (2D) analysis of the digital videos using the Kinovea® software (0.8.15 version, England). The peak of pelvic posterior rotation during the 10s of the bridge test was the greatest degree of the angle formed by a line connecting the anterior superior iliac spines and a horizontal line on the pelvic transverse plane (Fig. 2).10 In a pilot study with 8 participants and two days of data collection seven days apart, this test presented excellent test-retest reliability (intraclass correlation coefficient – ICC3,3=0.95; 95% CI: 0.75, 0.98), with standard error of measurement of 1.77° and minimal detectable change of 2.5°.
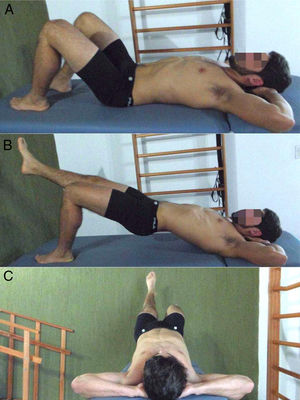
A handheld dynamometer (microFET2; Hoggan Scientific, LLC, Salt Lake City UT, USA) was used to measure the isometric strength of the trunk and hip muscles. To evaluate the strength of the trunk rotators, the participant remained in supine position with the trunk supported by a foam wedge (50cm×50cm×30cm), arms crossed on the chest, knee flexed and supported by a half-cylinder pillow. This test position was adapted from a previous study17 in order to allow the participant to isometrically rotate the trunk. The examiner positioned the dynamometer on the anterior surface of the acromion of the non-dominant side and fixed it with a rigid strap. The participant was instructed to perform maximal trunk anterior rotation toward the contralateral side (i.e. dominant side raised during bridge test) (Fig. 3A).17 This test presented excellent test-retest reliability (ICC3,3=0.93; 95% CI: 0.55, 0.99), with standard error of measurement of 26.5N and minimal detectable change of 73.1N.
To evaluate the isometric strength of the trunk extensors, the participant was in prone position, with the arms by the side and elbows extended. The dynamometer was positioned between the superior angles of the scapulas and fixed by a rigid strap (Fig. 3B).18 In addition, the pelvis of the participant was fixed to the treatment table by another rigid strap. The participant was instructed to lift the arms, head and trunk from the treatment table and push back against the dynamometer as hard as possible until the examiner said stop. This test presented excellent test-retest reliability (ICC3,3=0.91; 95% CI: 0.70, 0.98), with standard error of measurement of 10.8N and minimal detectable change of 29.9N.
To evaluate the isometric strength of the hip internal and external rotators of the non-dominant side (support limb during bridge test), the participant was in prone position with the knee of the side being evaluated flexed by 90° and the contralateral knee extended. We also used a rigid strap to stabilize the pelvis of the participant on the treatment table during the test. To assess hip internal rotators strength, the dynamometer was positioned on the lateral aspect of the shank, five centimeters proximal to the lateral malleolus (Fig. 3C). The participant was instructed to execute maximal strength in the direction of hip internal rotation. This test presented excellent test-retest reliability (ICC3,3=0.80; 95% CI: 0.48, 0.95), with standard error of measurement of 14.3N and minimal detectable change of 39.4N. In order to assess hip external rotators strength, the dynamometer was positioned on the medial aspect of the shank, five centimeters proximal to the medial malleolus (Fig. 3D).19 The participant was instructed to execute maximal strength in the direction of hip external rotation. This test presented excellent test-retest reliability (ICC3,3=0.89; 95% CI: 0.66, 0.97), with standard error of measurement of 11.6N and minimal detectable change of 32.0N.
To evaluate the non-dominant hip extensors strength, the participant was in prone position with the knee of the side being evaluated flexed by 90° and the contralateral knee extended. The dynamometer was positioned on the distal region of the femur and fixed by a strap.19 In addition, a rigid strap fixed the pelvis of the participant on the treatment table (Fig. 3E). The participant was instructed to push trying to move the foot toward the ceiling with maximal effort. This test presented excellent test–retest reliability (ICC3,3=0.91; 95% CI: 0.62, 0.98), with standard error of measurement of 24.2N and minimal detectable change of 66.8N.
To evaluate non-dominant hip abductors strength, the participant was positioned in side lying, arms in front of the body, trunk stabilized by a rigid strap and hip positioned in neutral abduction and extension. The dynamometer was positioned five centimeters above the femur lateral epicondyle (Fig. 3F).20 The participant was instructed to push trying to move the leg up with maximal effort. This test presented excellent test-retest reliability (ICC3,3=0.95; 95% CI: 0.76, 0.98), with standard error of measurement of 21.6N and minimal detectable change of 59.6N.
For all the strength tests, the participant performed one familiarization trial. Then, the participant performed maximal muscle isometric contractions for five seconds. This procedure was repeated three times, with intervals of 15s between trials, and the examiner provided verbal encouragement to promote maximal effort by the participants. The order of the tests was randomized. The strength variables were reported in newtons (N). One examiner performed the bridge test and another examiner performed the muscle strength measures and they were both blinded to each other test values.
Statistical analysisDescriptive statistics were performed for all of the variables. The magnitude of pelvic posterior rotation data were tested for normal distribution using the Shapiro–Wilk test and presented normal distribution. Multiple linear regression analysis using the forced entry procedure was performed to identify if strength variables could predict pelvic posterior rotation during the bridge test. The low correlations between the muscle strength variables (i.e. r>0.8) and the variance inflation factors lower than 10 minimized the effects of multicollinearity in the regression model.21 In addition, the assumptions of normality and homoscedasticity of residuals were tested. The significance was set at α=0.05. SPSS 14.0 software (SPSS Inc., Chicago, IL) was used for all analyses. The power of the multiple linear regression analysis was evaluated in G*Power software.22
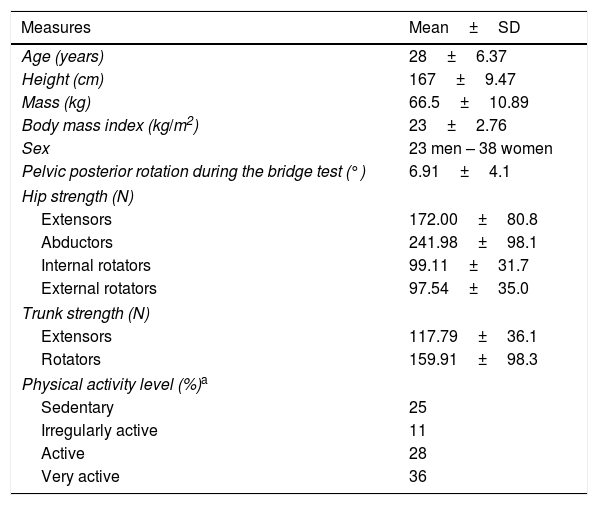
ResultsTable 1 presents the participants’ characteristics, the pelvic posterior rotation during the bridge test with unilateral knee extension and muscle strength data.
Participants’ characteristics, pelvic posterior rotation during the bridge test and muscle strength data.
| Measures | Mean±SD |
|---|---|
| Age (years) | 28±6.37 |
| Height (cm) | 167±9.47 |
| Mass (kg) | 66.5±10.89 |
| Body mass index (kg/m2) | 23±2.76 |
| Sex | 23 men – 38 women |
| Pelvic posterior rotation during the bridge test (°) | 6.91±4.1 |
| Hip strength (N) | |
| Extensors | 172.00±80.8 |
| Abductors | 241.98±98.1 |
| Internal rotators | 99.11±31.7 |
| External rotators | 97.54±35.0 |
| Trunk strength (N) | |
| Extensors | 117.79±36.1 |
| Rotators | 159.91±98.3 |
| Physical activity level (%)a | |
| Sedentary | 25 |
| Irregularly active | 11 |
| Active | 28 |
| Very active | 36 |
Abbreviations: cm, centimeters; kg, kilograms; m, meters; SD, standard deviation; N, newtons.
The regression model revealed that muscle strength predicted pelvic posterior rotation during the bridge test with unilateral knee extension (r=0.54; p=0.003). Specifically, strength of the trunk rotators and hip internal rotators predicted reduced magnitude of pelvic posterior rotation. In addition, hip extensors strength predicted increased magnitude of pelvic posterior rotation. Table 2 presents the results of the multiple linear regression model. The regression model had a power of 97%.
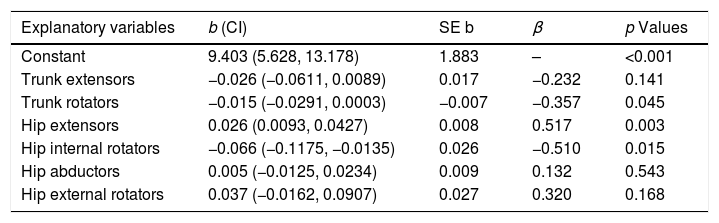
Multiple linear regression model results.
| Explanatory variables | b (CI) | SE b | β | p Values |
|---|---|---|---|---|
| Constant | 9.403 (5.628, 13.178) | 1.883 | – | <0.001 |
| Trunk extensors | −0.026 (−0.0611, 0.0089) | 0.017 | −0.232 | 0.141 |
| Trunk rotators | −0.015 (−0.0291, 0.0003) | −0.007 | −0.357 | 0.045 |
| Hip extensors | 0.026 (0.0093, 0.0427) | 0.008 | 0.517 | 0.003 |
| Hip internal rotators | −0.066 (−0.1175, −0.0135) | 0.026 | −0.510 | 0.015 |
| Hip abductors | 0.005 (−0.0125, 0.0234) | 0.009 | 0.132 | 0.543 |
| Hip external rotators | 0.037 (−0.0162, 0.0907) | 0.027 | 0.320 | 0.168 |
Abbreviations: b, unstandardized coefficients; CI, confidence interval; SE b, standard error; β, standardized coefficients.
This study demonstrated that strength of the trunk and hip muscles predicted part of the variability in pelvic posterior rotation during the bridge test with unilateral knee extension (i.e. core stability). More specifically, strength of the hip internal rotators and trunk rotators predicted reduced magnitude of pelvic posterior rotation during the test, which is in accordance with our initial hypothesis. However, strength of the hip extensors predicted increased magnitude of pelvic posterior rotation, which was not expected. Finally, trunk extensors and hip abductors and external rotators did not predict the performance during the bridge test.
The association between strength of the hip internal rotators and reduced magnitude of pelvic posterior rotation during the bridge test may be explained by the relationship between these muscles line of action23 and hip movement during the bridge test. During this test, as the pelvis posteriorly rotates, the hip of the support limb externally rotates.24 Therefore, action of the hip internal rotators reduces hip external rotation angles23 and consequently reduces magnitude of pelvic posterior rotation. This result suggests that individuals with increased pelvic posterior rotation during the bridge test (i.e. poor core stability) might also have weak hip internal rotators. In addition, this finding may help to explain the relationship between hip internal rotators weakness and chronic hip joint pain,25 since poor core stability,26 along with increased pelvic motion during different tasks27 may overload the hip joint. Future studies should investigate if strengthening of the hip internal rotators28 reduces pelvic rotation during the bridge test and consequently improves core stability.
Strength of the trunk rotators predicted reduced magnitude of pelvic posterior rotation during the test. Trunk rotators are also pelvic anterior rotators,29 especially when the trunk is fixed and the pelvis is not, as in the bridge test with unilateral knee extension. Therefore, the trunk rotators act as pelvic anterior rotators30 and consequently reduce the magnitude of pelvic posterior rotation during the bridge test. In clinical settings, individuals with poor core stability might benefit from trunk rotators strengthening. In addition, this result may explain the relationship between weakness of abdominal oblique muscles and different injuries, such as osteitis pubis.31 In fact, a recent study demonstrated that a nonoperative rehabilitation program including core stability training reduced pain and allowed return to training in soccer players with pubic stress syndrome with no recurrence after two years.32
Hip extensors strength predicted increased magnitude of pelvic posterior rotation during the bridge test. Gluteus maximus is a hip extensor that is recruited to maintain hip extension of the support limb during the bridge test.33 However, gluteus maximus also externally rotates the hip. Therefore, gluteus maximus recruitment to maintain the hip in neutral position in the sagittal plane might have resulted in increased hip external rotation (i.e. increased pelvic posterior rotation) in individuals with stronger hip extensors. The relationship between hip extensors strength and core stability needs more scientific investigation. Hip extensors are highly active during the bridge test with unilateral knee extension.34 Therefore, their weakness may predict other parameters related to better performance of this test, such as increased maximal endurance time and lower perceived exertion.34
This study had some limitations. First, maximal isometric muscle strength might not be the best measure of trunk and hip muscles’ function. However, the bridge test with unilateral knee extension is a quasi-static test and we evaluated isometric strength with the muscles at lengths similar to the muscles’ lengths assumed during the bridge test. Future studies should investigate the relationship between core stability and different muscle functions, such as concentric and eccentric strength,35 power, rate of force development36 and endurance. Second, our sample had different levels of physical activity, which may influence the relationship between core muscles’ strength and core stability. Although having individuals with different physical activity levels increased the external validity of this study, future studies with more homogeneous sample may find different results. Finally, we did not control for variations between the three repetitions of muscle strength measurement.37 However, muscle strength measurements presented excellent reliability in the pilot study.
ConclusionsThe hip internal rotators and trunk rotators isometric strength predicted reduced magnitude of pelvic posterior rotation during the bridge test with unilateral knee extension. In addition, the hip extensors isometric strength predicted increased magnitude of pelvic posterior rotation during the same test. Hip abductors, external rotators and trunk extensors isometric strength did not predict performance during the bridge test. These results suggest that individuals with poor performance during the bridge test with unilateral knee extension have weak hip internal rotators and weak trunk rotators. Therefore, physical therapists should properly evaluate strength of the hip internal rotators and extensors and trunk rotators in individuals presenting poor performance during the bridge test.
Conflicts of interestThe authors declare no conflicts of interest.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001. We are also thankful to the State of Minas Gerais Funding Agency FAPEMIG [grant numbers APQ-01017-17 and APQ 00712-15].